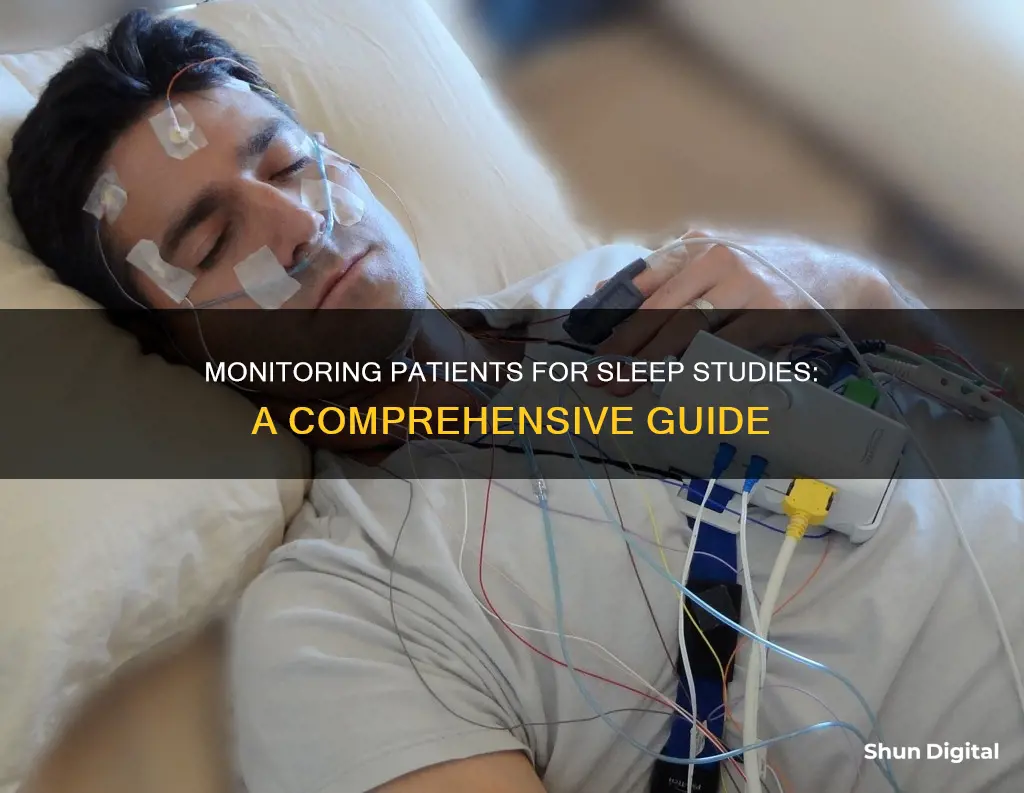
Sleep studies are a common diagnostic test that can help identify sleep disorders and issues. They involve recording multiple systems in the body while a patient sleeps, including brain activity, eye movement, heart function, and breathing. This data helps healthcare providers understand a patient's unique sleep patterns and identify any disruptions or disorders. The test is painless and typically takes one night to complete, with sensors attached to the patient's head and body to monitor their sleep. Sleep studies are an important tool to diagnose and treat conditions like sleep apnea, restless leg syndrome, and other sleep-related issues.
| Characteristics | Values |
|---|---|
| Purpose | To help diagnose and treat a variety of sleep disorders, including sleep apnea, restless legs syndrome, and certain causes of excessive sleepiness |
| Type of study | Polysomnography |
| Location | Sleep lab or clinic that resembles a comfortable hotel room |
| Timing | Usually overnight during normal sleeping hours, but can be scheduled during the day for those who work night shifts |
| Sensors | Electroencephalography (EEG), Electrocardiography (EKG or ECG), Electromyogram (EMG), Electro-oculography (EOG), breathing sensors, RIP belt, pulse oximeter |
| Video and Audio Monitoring | Yes, to observe and record the patient's movements and behaviours during sleep |
| Preparation | Avoid caffeine, alcohol, and naps on the day of the study; bring comfortable clothing and personal items |
| Duration | One night, but may be extended for multiple nights in certain cases |
| Results | Interpreted by a healthcare provider and shared with the patient within a few days to weeks |
What You'll Learn
- Sensors are attached to the patient's head and body to monitor brain activity and other data
- The patient sleeps while being monitored by a technician.
- The technician will adjust sensors if they come loose
- The patient can be woken up by the technician if there are signs of a serious problem
- The sensors are removed in the morning and the results are sent to a doctor for interpretation

Sensors are attached to the patient's head and body to monitor brain activity and other data
EEGs are coated with a sticky, electrically conductive gel that helps them adhere to the patient's head. These sensors detect and record electrical activity in the brain, which occurs in different wave types during various sleep stages. This data is crucial for identifying sleep disorders and issues.
In addition to the sensors, elastic belts may be wrapped around the patient's chest and abdomen to measure breathing. A clip may also be placed on the patient's finger or earlobe to monitor oxygen levels in the bloodstream. These sensors and belts allow healthcare providers to gain a comprehensive understanding of the patient's sleep quality and identify any potential sleep disorders or issues.
The data collected during a sleep study is then interpreted by a healthcare provider, who can determine if there are any medical issues and make a diagnosis. This process usually takes a few days, and the results are discussed with the patient during a follow-up visit.
Best 1440p Monitors: Elevate Your Viewing Experience
You may want to see also

The patient sleeps while being monitored by a technician.
The patient will be attached to various sensors that monitor their sleep. These include electroencephalography (EEG) sensors, which are coated in a sticky, electrically conductive gel that helps them stay attached to the patient's head. There are also electrocardiography (EKG or ECG) sensors, electromyography (EMG) sensors, and electro-oculography (EOG) sensors. Additionally, there are breathing sensors, a respiratory inductive plethysmography (RIP) belt, and a pulse oximeter. All of these sensors work together to provide a comprehensive view of the patient's sleep quality.
The technician will be on hand to monitor the patient's sleep and record the results of the test. They will also assist the patient with any issues that may arise during the night. If a sensor comes loose, the technician will wake the patient and reattach it. The technician will also check on the patient if they observe any signs of a serious problem, such as a seizure or other potential medical emergency.
The sleep study ends when the patient wakes up in the morning and the sensors are removed. The data collected during the study will then be reviewed and interpreted by a healthcare provider, who will determine if the patient has a medical issue and make a diagnosis.
Enhancing Your Car's Safety: Adding Blind Spot Monitoring
You may want to see also

The technician will adjust sensors if they come loose
During a sleep study, a technician will attach sensors to your head and body with adhesive. The sensors are connected to a computer by wires, which are gathered over your head to allow you to move around during sleep. If a sensor comes loose during the night, the technician will come into the room to reattach it. This is usually done without waking the patient if possible.
The wires connecting the sensors are long enough to allow the patient to move comfortably in bed. However, if the patient needs to get out of bed, a staff member may need to assist with unplugging the wires. The patient should not unplug them without being instructed to do so by a staff member, as this could affect the results of the sleep study.
The sensors are attached to the body using medical tape and/or paste. In rare instances, some people with sensitive skin may develop local irritation at the electrode sites. If you have experienced skin irritation due to EKG testing in the past, or have an adhesive allergy, you should notify the sleep centre and the technologist prior to the study.
The sensors are not painful, but removing them may cause mild discomfort. Staff can help minimise or prevent this when the study is over.
Monitoring Folder Sizes: Strategies for Effective Data Management
You may want to see also

The patient can be woken up by the technician if there are signs of a serious problem
Sleep studies are diagnostic tests that monitor a patient's brain, heart, and respiratory activity while they sleep. The patient is connected to various sensors that monitor their body's activity, and the data is recorded and interpreted by a healthcare provider. This data helps providers diagnose and treat various sleep disorders, including sleep apnea and restless leg syndrome.
During a sleep study, a technician will monitor the patient's sleep from a nearby room. If there are any signs of a serious problem, such as a seizure or other potential medical emergency, the technician may wake the patient. This is done to ensure the patient's safety and well-being.
The decision to wake a patient during a sleep study is not taken lightly, as it may impact the data collection process. However, the patient's health and safety are always the top priority. In most cases, the technician will only intervene if there are clear indications of a potential medical emergency.
It is important to note that sleep studies are generally very safe, and side effects or complications are rare. The most common issue is mild irritation from the adhesives used to attach the sensors. The sleep lab staff are trained to handle any potential issues that may arise during the study and will provide assistance as needed.
Overall, the patient's comfort and safety are of utmost importance during a sleep study. While it is uncommon for a patient to be awakened, the technician will intervene if there are any signs of a serious problem to ensure the patient's well-being.
Dismantling Your Acer Predator Monitor and Stand Safely
You may want to see also

The sensors are removed in the morning and the results are sent to a doctor for interpretation
The sleep study, or polysomnography, is a diagnostic test that involves recording multiple systems in the body while the patient sleeps. The test is performed by medical technicians, technologists, assistants, and nurses. Sensors are placed on the patient's head and body to record brain activity and gather information from the body. These sensors are removed in the morning when the patient wakes up.
The sensors used during a sleep study include:
- Electroencephalography (EEG) sensors, which are coated with a sticky, electrically conductive gel that helps them stick to the patient's head and detect brain waves.
- Electrocardiography (EKG or ECG) sensors, which are placed on the chest to monitor the electrical activity of the heart.
- Electromyogram (EMG) sensors, which are attached to the skin on the face and leg to track muscle movement.
- Electro-oculography (EOG) sensors, which are placed around the eyes to detect eye movement.
- Breathing sensors, which detect air movement through the mouth and nose.
- Respiratory inductive plethysmography (RIP) belt, which detects the expansion of the torso during breathing.
- Pulse oximeter, a small adhesive sensor that is placed on the tip of the index finger to read the patient's pulse and blood oxygen levels.
After the sleep study, a healthcare provider will interpret the data gathered from these sensors. This interpretation is crucial as it allows the provider to identify any medical issues and make a diagnosis. The provider will then contact the patient to discuss the findings and recommend next steps, which may include a follow-up visit to go over the results in more detail and determine treatment options.
The results of a sleep study can help diagnose various sleep disorders, including sleep apnea, restless leg syndrome, and other disruptive sleep disorders. The data provides a detailed picture of the patient's unique sleep patterns, including the time spent in light and deep sleep stages, oxygen levels, and how often the patient awakens.
Monitoring Android App Performance: A Comprehensive Guide
You may want to see also
Frequently asked questions
A sleep study is a diagnostic test that involves recording multiple systems in the body while the patient sleeps. This includes monitoring the brain, heart, and respiratory system.
A sleep study helps healthcare providers diagnose or rule out health issues related to sleep. It is often recommended when a patient exhibits symptoms of conditions that affect sleep quality.
The patient will be asked to spend the night in a sleep lab, where technicians will attach sensors to their head and body to monitor their brain activity and other physiological parameters. The patient will then be allowed to sleep, and the technicians will monitor the data.
It is recommended to follow your usual daily routine and avoid caffeine in the afternoon and evening. Bring comfortable sleepwear, toiletries, and something to keep you occupied before sleeping, such as a book.
The sensors will be removed when you wake up. The data collected during the study will be analysed, and the results will be shared with you and your doctor to determine the next steps in your care.