ACE inhibitors are a medication class used to treat and manage hypertension, a significant risk factor for coronary disease, heart failure, stroke, and other cardiovascular conditions. They are one of the most widely prescribed drugs in general practice for the treatment of hypertension.
ACE inhibitors are also one of the most frequent drugs associated with preventable drug-related morbidity incidents. There are guidelines in place regarding the monitoring of renal function during treatment with these drugs.
Monitoring of ACE inhibitors includes checking blood pressure, electrolytes, renal function, and glomerular filtration rate.
| Characteristics | Values |
|---|---|
| Indications | Hypertension, Systolic Heart Failure, Chronic Kidney Disease, Post Myocardial Infarction |
| Contraindications | Hypersensitivity, Pregnancy, Abnormal Renal Function, Aortic Valve Stenosis, Hypovolemia |
| Adverse Effects | Dry Cough, Angioedema, Hyperkalemia, Increased BUN and Creatinine, Hypotension, Dizziness |
| Monitoring | Renal Function, Blood Urea Nitrogen, Serum Creatinine, Electrolytes (Potassium), Glomerular Filtration Rate |
What You'll Learn

Monitor blood pressure
Monitoring blood pressure is an important part of ACE inhibitor usage. Blood pressure should be checked within 3 months of the initiation of ACE inhibitors, and regularly thereafter.
In one study, 94.8% of patients had their blood pressure checked within 3 months of starting ACE inhibitors, and 91.2% of patients had their blood pressure checked between January 2010 and June 2011.
According to the UK's National Institute for Health and Care Excellence (NICE), baseline blood pressure testing is recommended when initiating ACE inhibitors in patients with hypertension, heart failure, myocardial infarction, or chronic kidney disease. NICE also recommends follow-up blood pressure monitoring within 2 weeks of treatment initiation for patients with heart failure, myocardial infarction, and chronic kidney disease.
For patients with heart failure, NICE recommends ongoing blood pressure monitoring at 1, 3, 6, and 12 months after the first retest.
In addition to monitoring blood pressure, it is important to monitor renal function and serum potassium levels when taking ACE inhibitors. This includes measuring creatinine and glomerular filtration rate.
ACE inhibitors are widely prescribed and effective in treating hypertension, but proper monitoring is crucial to ensure their safe and effective use.
Hotels and Internet Privacy: Monitoring Guest Online Activity
You may want to see also

Monitor renal function
Monitoring renal function is critical when using ACE inhibitors, as they can cause a sudden decline in kidney function. This is usually reversible, but if not identified early, it can lead to acute renal failure.
To prevent this, it is recommended that serum creatinine and potassium levels are monitored before and after initiating treatment with ACE inhibitors. This is especially important for patients with myocardial infarction, hypertension, or high baseline potassium levels, as they are at higher risk of a ≥30% increase in creatinine after ACE inhibitor initiation.
For patients with heart failure, it is recommended that serum creatinine and potassium levels are checked within two weeks of treatment initiation and then at least annually. For patients with myocardial infarction, at least annual monitoring is also recommended.
In addition, for patients with chronic kidney disease, it is recommended that renal function is checked within one week of initiation, after every increase in dosage, and then at least annually.
It is also important to monitor patients' blood pressure, as a sudden drop can lead to renal failure.
Water Usage Monitoring in California: How Does It Work?
You may want to see also

Monitor electrolytes
Electrolytes should be checked before starting ACE inhibitor treatment, and then again 1–2 weeks later, and after each dose increment. A decrease in the estimated glomerular filtration rate (eGFR) and an increase in creatinine often occur with ACE inhibitors, so these should be monitored. The drugs may need to be discontinued if the eGFR decreases by more than 15%, if creatinine increases by more than 20%, or if hyperkalaemia develops.
In one study, 37.1% of patients had their electrolytes checked within three months of initiation, and 73% within 18 months. In another study, 10% of patients had neither baseline nor follow-up monitoring of creatinine within 12 months before and two months after initiation of an ACE inhibitor, 28% had monitoring only at baseline, 15% only at follow-up, and 47% at both baseline and follow-up.
ACE inhibitors are contraindicated if the patient has a history of hypersensitivity to any ACE inhibitor, or component of the formulation, angioedema related to previous treatment with an ACE inhibitor, idiopathic or hereditary angioedema, or current use of aliskiren in a patient with diabetes mellitus.
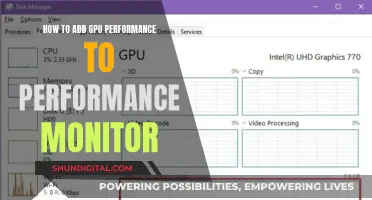
Unlocking GPU Usage Monitoring: A Unified Approach
You may want to see also

Monitor glomerular filtration rate
Monitoring glomerular filtration rate (GFR) is an important aspect of ACE inhibitor usage, especially in patients with chronic kidney disease or congestive heart failure (CHF). GFR is a measure of kidney function and can be estimated using an individual's age, gender, creatinine level, and race.
GFR monitoring is crucial as ACE inhibitors can cause a slight reduction in GFR when initiating therapy. This reduction is typically <10-20% and is a positive indicator that the drugs are having their desired effect. However, in certain cases, ACE inhibitors can lead to acute renal failure (ARF) or acute kidney injury, which is characterised by a sudden reduction in renal function and a rise in serum creatinine concentration.
ARF can occur when renal perfusion pressure cannot be sustained due to substantial decreases in mean arterial pressure (MAP) or when GFR becomes highly dependent on angiotensin II. It is more likely to occur in patients with the following conditions:
- Pre-existing hypotension and low cardiac filling pressures
- Extracellular fluid (ECF) volume depletion
- High-grade bilateral renal artery stenosis
- Stenosis of a dominant or single kidney, as in a renal transplant recipient
- Atherosclerotic disease in smaller preglomerular vessels
- Afferent arteriolar narrowing due to hypertension or chronic cyclosporine use
Additionally, the risk of ACE inhibitor-induced ARF is higher in patients with chronic renal insufficiency, and patients taking certain other medications, such as diuretics, non-steroidal anti-inflammatory drugs (NSAIDs), or cyclosporine.
To monitor GFR when using ACE inhibitors, it is recommended to evaluate serum creatinine and electrolyte levels before and one week after initiating therapy. A rise in serum creatinine of ≥0.5 mg/dL if the initial serum creatinine is <2.0 mg/dL, or ≥1.0 mg/dL if the baseline creatinine exceeds 2.0 mg/dL, should prompt consideration for stopping the medication and further renal evaluation.
It is important to note that a slight rise in serum creatinine is expected and not a reason to discontinue treatment unless one of the above-mentioned conditions is present. Monitoring should also include checking for hyperkalemia, especially in patients with diabetes or chronic renal failure, as ACE inhibitors can lead to a modest increase in plasma potassium levels.
Monitoring Employee Internet Usage: What Employers Can and Can't Do
You may want to see also

Monitor potassium levels
Monitoring potassium levels is an important aspect of ACE inhibitor usage, as these medications can cause hyperkalemia, or high potassium levels. This is due to the mechanism of ACE inhibitors, which block the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. By inhibiting angiotensin II, ACE inhibitors reduce blood pressure and decrease aldosterone secretion. Aldosterone is a hormone that increases sodium reabsorption and water reabsorption, which in turn leads to the secretion of potassium. Without aldosterone, potassium levels can rise.
It is recommended to check potassium levels before starting ACE inhibitors, as initiation is typically not appropriate if pre-treatment potassium levels are above 5.0 mmol/L. Potassium levels should also be checked 1-2 weeks after starting or changing the dose of an ACE inhibitor, and after each dose increment.
If potassium levels rise above 5.5 mmol/L, it is recommended to stop taking ACE inhibitors and seek specialist advice. For levels between 5.0-5.9 mmol/L, it is advised to review other potassium-sparing treatments and reduce the ACE inhibitor dose, with a review in 5-7 days. If hyperkalemia persists or becomes severe (above 6.0 mmol/L), it is important to stop taking ACE inhibitors and seek urgent clinical advice.
In addition to monitoring potassium levels, it is also crucial to monitor renal function, as a slight reduction in glomerular filtration rate (GFR) is common when initiating ACE inhibitor therapy. Patients with heart failure, chronic kidney disease, or bilateral renal artery stenosis with poor renal perfusion are at a higher risk of further reductions in GFR, which may require discontinuation of the ACE inhibitor.
Monitoring Resource Usage: Strategies for Optimal Performance
You may want to see also
Frequently asked questions
It is recommended that you get your blood pressure checked within 3 months of starting an ACE inhibitor.
It is important to get your electrolytes and renal function checked within 3 months of starting an ACE inhibitor.
Some common side effects of ACE inhibitors include dry cough, angioedema, dizziness, hypotension, increased BUN and creatinine, and hyperkalemia.
If you experience side effects from ACE inhibitors, consult your doctor. They may recommend discontinuing the medication or switching to an alternative treatment.