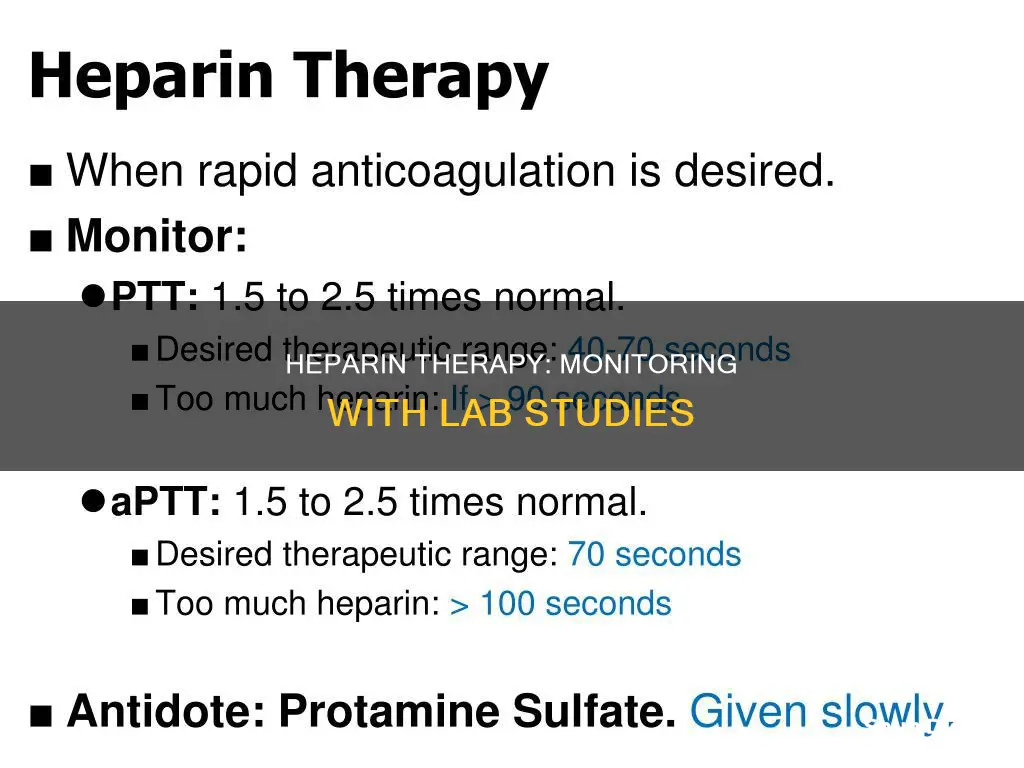
Heparin therapy is monitored using the activated partial thromboplastin time (aPTT) test, which measures the time required for a blood sample to form a clot. The aPTT test has been used to monitor the effects of heparin therapy since its introduction in 1953. However, the test has limitations and several factors can interfere with its accuracy, including physiological and pharmaceutical variables.
An alternative method for monitoring heparin therapy is the anti-factor Xa assay, which can monitor heparin and its low molecular weight heparin (LMWH) analogues. This method is not affected by oral anticoagulants or herbal supplements, which interfere with the aPTT test.
| Characteristics | Values |
|---|---|
| --- | --- |
| Correlation between POCT-APTT and lab-APTT | Strongly positive (rs = 0.77) |
| Correlation between POCT-APTT and anti-Xa activity | Weakly positive (rs = 0.46) |
| Inter-method agreement between POCT-APTT and lab-APTT | 0.27 |
| Inter-method agreement between POCT-APTT and anti-Xa activity | 0.30 |
| Median TAT from sample collection to lab delivery of results for lab-APTT | 50.9 min |
| Median TAT from sample collection to lab delivery of results for anti-Xa | 66.3 min |
| Median TAT from sample collection to POCT-APTT results | <5 min |
What You'll Learn

Activated partial thromboplastin time (aPTT)
The aPTT test is used to check for problems with a specific group of blood clotting factors. It can help find the cause of:
- Too much bruising or bleeding.
- Clotting problems, including certain autoimmune diseases such as lupus and antiphospholipid syndrome (APS).
- It is also used to monitor people taking heparin, a medicine used to prevent and treat blood clots, to ensure the dose is safe and effective.
- The risk of possible bleeding problems before surgery or medical procedures.
The aPTT test is considered a more sensitive version of the PTT test and is used to monitor the patient’s response to heparin therapy. The reference range for aPTT is 30-40 seconds, while for PTT it is 60-70 seconds.
The aPTT test evaluates factors I (fibrinogen), II (prothrombin), V, VIII, IX, X, XI and XII. It is a useful test as it can help diagnose a range of conditions, including:
- Congenital deficiencies of intrinsic system clotting factors such as factors VIII, IX, XI, and XII, including hemophilia A and hemophilia B.
- Congenital deficiency of Fitzgerald factor (prekallikrein).
- Von Willebrand disease, which is the most common inherited bleeding disorder, affecting platelet function due to decreased von Willebrand factor activity.
- Liver cirrhosis.
- Vitamin K deficiency.
- Disseminated intravascular coagulation (DIC).
- Heparin therapy.
- Coumarin therapy.
- Nonspecific inhibitors, such as lupus anticoagulant and anticardiolipin antibodies.
- Specific circulating anticoagulants, inhibitor antibodies that specifically target certain coagulation factors.
There are some factors that may interfere with the aPTT test, including certain drugs such as antihistamines, ascorbic acid, chlorpromazine, heparin, and salicylates. Additionally, an incorrect blood-to-citrate ratio, a highly increased or decreased hematocrit, and blood samples drawn from a heparin lock or a heparinized catheter can also interfere with the test.
Performance Monitoring: Essential for Business Success and Growth
You may want to see also

Anti-factor Xa assay
The anti-factor Xa assay is a functional assay that measures the activity of heparins in the blood. Heparin is a naturally occurring anticoagulant (blood thinner) that works by binding to antithrombin, a natural anticoagulant, and increasing its activity. This process slows coagulation by speeding up thrombin inactivation.
The anti-factor Xa assay is used to monitor the anticoagulant effects of heparin therapy and is considered the most accurate assay for monitoring unfractionated heparin (UFH). It can also monitor low-molecular-weight heparin (LMWH) and the newer generation of direct oral anticoagulants (DOACs).
The assay measures the ability of heparin to inhibit factor Xa by forming a complex with antithrombin. The complex inactivates factor Xa, and the amount of residual factor Xa is inversely proportional to the amount of heparin in the sample. This is done using a chromogenic procedure, where the residual factor Xa cleaves a chromophore-linked substrate, releasing a coloured compound that can be detected by a spectrophotometer. The intensity of the colour is inversely proportional to the amount of heparin in the sample, and results are compared to a standard curve.
The anti-factor Xa assay is particularly useful for monitoring LMWH, which has minimal effect on the activated partial thromboplastin time (aPTT), the test previously used to monitor heparin therapy. The anti-factor Xa assay is also unaffected by acute-phase reactions and most factor deficiencies, except antithrombin deficiency.
The therapeutic ranges for heparin are as follows:
- LMWH: 0.5-1.2 IU/mL
- UH: 0.3-0.7 IU/mL
The anti-factor Xa assay is indicated for monitoring heparin therapy in patients with renal dysfunction, those at extremes of weight, infants, pregnant women, and patients at high risk of thrombosis or bleeding, as well as those receiving prolonged treatment.
Asus Monitors: Anti-Glare or Not?
You may want to see also

Protamine titration
Protamine is a compound that can be used to neutralise heparin in vivo and in vitro. In vitro, protamine titration can be used to diagnose hemorrhagic states by measuring the amount of protamine required to neutralise heparin. The protamine equivalent varies depending on the heparin preparation and testing conditions.
In vivo, protamine is administered to patients to neutralise heparin and terminate its anticoagulant effects. The amount of protamine required depends on the heparin concentration in the patient's circulation, which is influenced by factors such as the time since heparin administration and the patient's hemodynamic and metabolic state. It is important to note that rapid injection of protamine can release histamine and cause platelet agglutination, leading to excessive bleeding.
Connecting Apple TV to a Monitor: A Simple Guide
You may want to see also

Thrombodynamics (TD)
The TD test is performed without mixing in a thin layer of plasma. The measurement cuvette with the blood plasma sample is placed inside a water thermostat. Clotting starts when an activator with immobilised tissue factor is immersed into the cuvette. The clot then propagates from the activating surface into the bulk of the plasma. The clot growth is registered via a CCD camera using a time-lapse microscopy mode in scattered light, and parameters of coagulation are calculated on a computer. The TD analyser T-2 device also supports the measurement of spatial dynamics of thrombin propagation during the process of clot growth via the usage of a fluorogenic substrate for thrombin.
The TD test has several advantages over other global methods of coagulation analysis. These include good standardisation, high reproducibility, independence of parameter values from patient age and gender, and a narrower parameter distribution in a normal population. These results indicate that TD is a promising universal assessment method that improves the quality of hemostasis analysis because it more reliably detects deviations from the parameters' reference values.
Monitor Smart TV Data Usage: Tips for Parents
You may want to see also

Activated clotting time (ACT)
The Activated Clotting Time (ACT) test is a point-of-care test (POCT) used to monitor the anticoagulant effect of unfractionated heparin (UFH) in patients undergoing cardio-pulmonary bypass, extracorporeal membrane oxygenation (ECMO), percutaneous transluminal coronary angioplasty, haemofiltration, or haemodialysis. The ACT test was first described by Hattersley in 1966 and came into clinical use in the mid-1970s.
The ACT test is performed by adding fresh, whole blood to a tube containing a negatively charged 'activator' such as celite, kaolin, or glass balls. This results in the formation of a clot. The type of activator affects the clotting time. The test is dependent on the presence of endogenous platelets as a source of phospholipid. The time taken for the clot to form is the ACT.
The ACT test is a rapid test that can be performed at the patient's bedside prior to surgery or other medical procedures. It can also be done in or near the operating room at intervals during and immediately after surgery. This type of testing is known as point-of-care testing. The ACT test allows for the measurement of relatively rapid changes in heparin infusion, helping to achieve and maintain a constant level of anticoagulation throughout the surgical or medical procedure.
The ACT test is preferred over laboratory tests due to its shorter time between sampling and results, smaller blood sample size, and reduced errors associated with sample mislabelling or mishandling. The ACT test is also useful when heparin is the only variable, but it becomes non-specific to heparin when other variables are altered.
The ACT test is influenced by a number of variables, including platelet count and function, the presence of a lupus anticoagulant, and certain medications such as aspirin and clopidogrel. The temperature of the blood may also affect ACT results, with hypothermia prolonging the ACT.
Detecting Keystroke Monitoring: What to Look For
You may want to see also
Frequently asked questions
The most common lab study used to monitor heparin is the activated partial thromboplastin time (aPTT) test.
The second most common lab study used to monitor heparin is the anti-factor Xa assay.
The third most common lab study used to monitor heparin is the prothrombin time (PT) test.
The least common lab study used to monitor heparin is the thrombodynamics (TD) test.
The gold standard for measuring heparin concentrations in plasma is protamine titration.