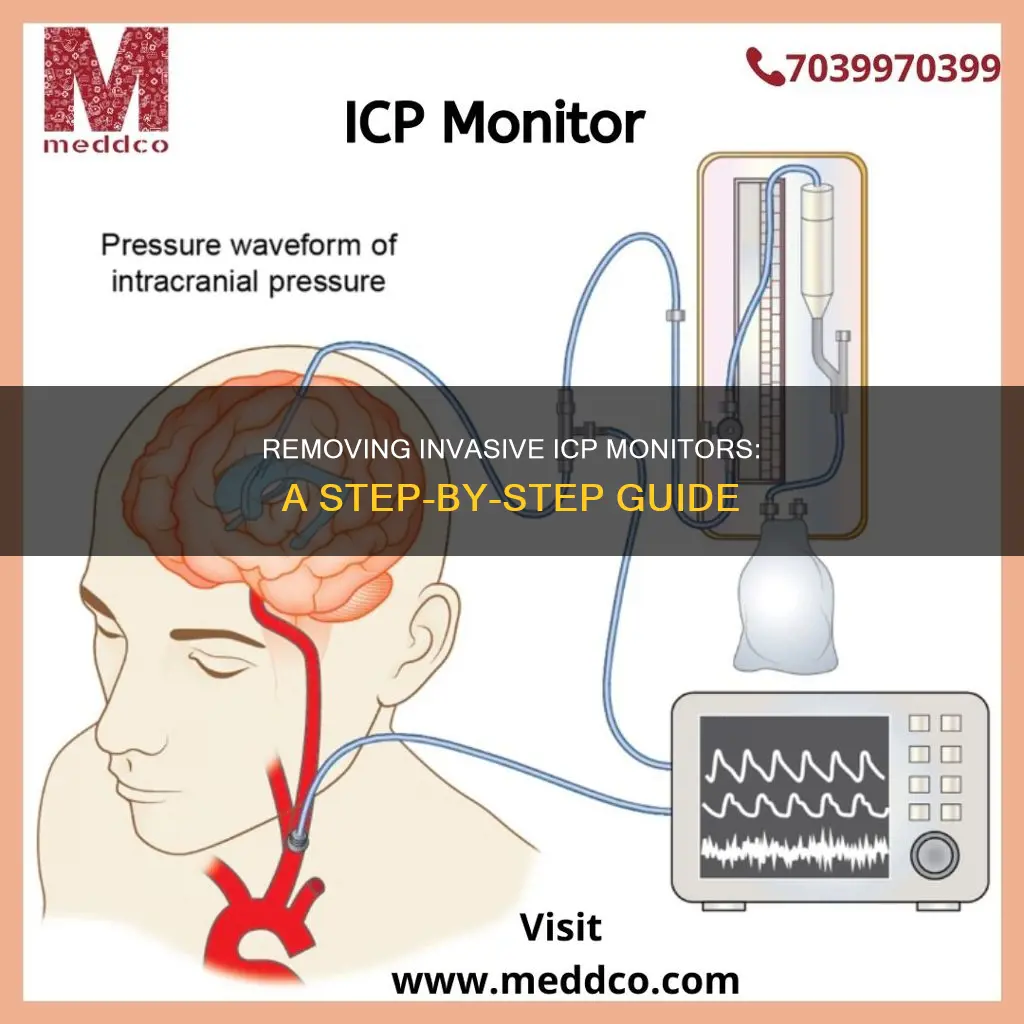
Intracranial pressure (ICP) monitoring is a procedure that involves inserting a device inside the skull to measure pressure. This procedure is typically performed on patients with life-threatening neurological emergencies, such as severe head injuries, brain tumours, or brain infections. The three main types of ICP monitors are the External Ventricular Drain (EVD), the Subarachnoid Bolt, and the Epidural Bolt. The choice of monitor depends on the specific clinical scenario and patient factors. While ICP monitoring provides valuable information for medical decision-making, it carries risks, including infection, bleeding, and cerebrospinal fluid (CSF) leakage.
| Characteristics | Values |
|---|---|
| Purpose | Measure pressure inside the skull |
| Monitoring methods | Intraventricular catheter, subdural screw (bolt), epidural sensor, lumbar catheter, intraparenchymal pressure microsensor |
| Procedure | A hole is drilled into the skull and a catheter or screw is inserted |
| Anaesthesia | Local or general |
| Preparation | Blood and urine tests, stop taking blood thinners, inform doctor of allergies to local anaesthetic |
| Risks | Brain herniation, brain injury, brain tissue damage, ventricular collapse, infection, bleeding, spinal fluid leak |
| Results | Analysed by a doctor, can take up to a week |
What You'll Learn

How to prepare for ICP monitoring
Intracranial pressure (ICP) monitoring is a diagnostic test that helps doctors determine whether high or low cerebrospinal fluid (CSF) pressure is causing your symptoms. The test involves inserting a small pressure-sensitive probe through the skull to directly measure the pressure in your head. Here are some essential steps and considerations to prepare for ICP monitoring:
- Understanding the Procedure: It is important to understand why ICP monitoring is necessary. ICP monitoring is often recommended for individuals with life-threatening neurological emergencies, severe head injuries, brain or nervous system diseases, and post-surgical complications. The procedure can help detect intense head pressure and abnormal CSF pressure, which may occur only during sleep.
- Medical History and Medication Review: Inform your doctor about any medical problems or allergies you may have. Provide a list of all the medications you are currently taking, including blood thinners, antiplatelet agents, and anticoagulants. It is crucial to discuss stopping or adjusting these medications with your doctor before the procedure.
- Consent and Risks: Your doctor will explain the procedure in detail, address any concerns you may have, and obtain your informed consent by asking you to sign a consent form. It is important to understand the risks associated with ICP monitoring, which include infection, bleeding, and potential complications such as brain herniation or injury.
- Pre-Procedure Testing: You will undergo a series of tests, including blood and urine tests, 3-7 days before the procedure. These tests help ensure that you are in a stable condition to undergo ICP monitoring and reduce the risk of infection or bleeding complications.
- Anesthesia and Fasting: ICP monitoring is usually performed under general anesthesia, so your doctor will provide instructions on fasting and other pre-anesthesia protocols.
- Sleep Apnea Equipment: If you have been prescribed equipment or devices for sleep apnea, bring them to the hospital unless you are undergoing skull base surgery.
- Skin Preparation: On the day of the procedure, your scalp will be cleaned and prepared with an antiseptic solution to reduce the risk of infection.
- Monitoring and Recording: During and after the procedure, your vital signs and neurological status will be closely monitored. It is important to notify the nurse of any adjustments to your head position, as this can affect CSF pressure measurements.
- Post-Procedure Care: After ICP monitoring, you will be moved to the intensive care unit for observation. Follow your doctor's instructions on activity restrictions, such as avoiding heavy lifting or straining, and refrain from swimming or bathing for the first week.
- Infection and Complication Vigilance: Be vigilant for signs of infection, such as fever, headache, neck stiffness, nausea, or vomiting. Report any symptoms or concerns to your medical team promptly.
- Follow-up and Results: After ICP monitoring, your doctor will analyze the data and combine it with other test results, such as eye examinations, MRI or CT scans, to determine the best course of treatment. This process may take up to a week, and complex cases may require further discussion at a case conference.
Remember to follow your doctor's specific instructions and guidelines for preparing for ICP monitoring, as they may vary based on your individual circumstances and the medical facility's protocols.
Opening an Acer LCD Monitor: A Step-by-Step Guide
You may want to see also

How to place an intraparenchymal pressure microsensor
The intraparenchymal pressure microsensor is a device used to measure intracranial pressure (ICP) and is generally placed when there is concern over elevated ICP. The procedure is usually carried out by a neurosurgeon in an operating room under general anaesthesia.
Firstly, the patient's scalp will be cleaned with an antiseptic solution and a small hole will be drilled into the skull. A small, calibrated pressure microsensor will then be passed through the hole and a short distance into the brain.
Once the patient wakes up, they may feel the normal side effects of anaesthesia, as well as some discomfort at the site of the probe placement. The patient will then be taken to the intensive care unit for monitoring.
The pressure probe is then connected to the ICP recording system, and intracranial pressure is measured continuously. To accurately measure CSF pressure, the patient must notify the nurse whenever they adjust the head of the bed elevation and always call for assistance when getting up to use the bathroom.
Infection and Bleeding Risks
Infection and bleeding are potential risks of the procedure. There is a 2-4% risk of infection, and while bleeding during the procedure is minimal, there is a very small risk of bleeding in the brain during the placement of the probe.
Simple Ways to Check Your Monitor's 155Hz Refresh Rate
You may want to see also

How to place a lumbar catheter
To place a lumbar catheter, the patient will first be scheduled for a series of tests 3 to 7 days in advance. These include blood and urine tests to ensure the patient does not have an infection or a tendency to bleed. It is also important that the patient has stopped taking any blood thinners after discussion with their doctor.
On the day of the procedure, the patient will be given an injection of antibiotics in their arm to reduce the risk of infection. They will then be asked to sit in a special chair or lie down on one side of the bed. The practitioner will mark the area on the patient's lower back where the spinal needle is to be placed and clean the area with a solution. The patient will then be injected with medicine to numb the skin on their lower back.
Once the skin is numb, the practitioner will insert the spinal needle into the marked area and direct it toward the spinal canal. The patient will feel pressure as the needle is put in place and should inform the doctor if they feel a sharp pain so that more numbing medicine can be administered.
The surgeon will then insert a catheter (a flexible tube) through the needle and then remove the needle, leaving the catheter in place. The catheter will be gently bandaged to the skin and connected to a device that measures the cerebrospinal fluid (CSF) pressure over a 24- to 72-hour period.
After the procedure, the patient should avoid straining or lifting heavy weights for 1 week, as well as swimming or bathing. They should also be aware of possible signs of delayed infection and contact their provider or go to the emergency room if these occur.
Finding the Ideal Monitor Size for 1440p Resolution
You may want to see also

How to remove an ICP monitor
Overview
Intracranial pressure (ICP) monitoring uses a device placed inside the head to measure the pressure inside the skull. This procedure is typically performed on patients with life-threatening neurological emergencies, such as severe head injuries, brain infections, or brain tumours.
There are three main types of ICP monitors: the intraventricular catheter, the subdural screw (or bolt), and the epidural sensor. The removal process for each type of ICP monitor will vary slightly, as described below.
Intraventricular Catheter Removal
The intraventricular catheter is inserted through a hole drilled in the skull and into the lateral ventricle of the brain. To remove the catheter, the following steps should be performed:
- Ensure that the patient is comfortably sedated or under general anesthesia.
- Remove any dressings or bandages covering the insertion site.
- Using sterile techniques, gently disconnect the catheter from the recording device.
- Slowly and carefully withdraw the catheter from the patient's brain and skull, following the same path it was inserted through.
- Apply gentle pressure to the insertion site to control any bleeding.
- Dress the insertion site with sterile gauze and secure it in place.
- Monitor the patient closely for any signs of increased ICP or other complications.
Subdural Screw (Bolt) Removal
The subdural screw is inserted through a drilled hole in the skull and into the subdural space between the skull and the dura mater. To remove the screw:
- Ensure the patient is sedated or under general anesthesia.
- Remove any dressings or bandages covering the insertion site.
- Using sterile techniques, carefully loosen and remove the screw, following the same path it was inserted.
- Apply gentle pressure to the insertion site to control any bleeding.
- Dress the insertion site with sterile gauze and secure it in place.
- Monitor the patient for increased ICP or other complications.
Epidural Sensor Removal
The epidural sensor is placed between the skull and the dural tissue through a hole drilled in the skull. To remove the sensor:
- Ensure the patient is sedated or under anesthesia.
- Remove any dressings or bandages.
- Using sterile techniques, carefully disconnect the sensor from the recording device.
- Slowly withdraw the sensor through the drilled hole, following the path of insertion.
- Apply gentle pressure to the insertion site to control any bleeding.
- Dress the insertion site with sterile gauze.
- Monitor the patient for increased ICP or other complications.
Post-Removal Care
After removing any type of ICP monitor, it is important to monitor the patient closely for complications such as increased ICP, bleeding, or infection. The patient may also experience headaches, dizziness, or lightheadedness, which can be managed with pain medication and increased fluid intake.
In some cases, a simple stitch may be required to close the wound and prevent cerebrospinal fluid (CSF) leakage. If signs of infection or other complications develop, the patient should seek immediate medical attention.
Best Places to Buy an Alexa Monitor
You may want to see also

ICP monitoring risks
Intracranial pressure (ICP) monitoring is a procedure that involves placing a device inside the head to measure the pressure inside the skull. While this procedure is often carried out on patients with life-threatening neurological emergencies, it is not without risks.
The risks associated with ICP monitoring include:
Brain herniation or injury
Increased intracranial pressure can lead to brain herniation, which occurs when the brain shifts or moves downwards towards the spinal column. This can cause compression of vital structures and can be life-threatening.
Damage to brain tissue
The insertion of the ICP monitor involves drilling a hole in the skull and inserting a catheter or screw into the brain. This procedure carries a risk of damaging delicate brain tissue, which could lead to permanent neurological deficits.
Inability to find the ventricle and place the catheter
In some cases, especially when the intracranial pressure is high, it may be difficult to insert the catheter into the lateral ventricle. This can result in unsuccessful ICP monitoring.
Risks of general anesthesia
General anesthesia is often used during the ICP monitoring procedure. As with any surgical procedure, there are risks associated with general anesthesia, including respiratory depression, allergic reactions, and cardiovascular complications.
Infection
The introduction of foreign objects and the creation of an entry point for bacteria increase the risk of infection. In the case of ICP monitoring, this could lead to meningitis, ventriculitis, or wound infection.
Intracranial haemorrhage
Drilling a hole in the skull and inserting a catheter carries a risk of intracranial haemorrhage, which can be life-threatening.
Device malfunction or difficulty with placement
ICP monitoring devices may malfunction or be difficult to place correctly, leading to inaccurate readings or the need for additional procedures.
Ventricular collapse
In rare cases, ventricular collapse can occur, leading to tentorial herniation and further complications.
Asus VG259: Monitor Camera Specs and Features Explored
You may want to see also
Frequently asked questions
Intracranial Pressure (ICP) monitoring uses a device placed inside the head to measure pressure inside the skull. There are two main ways to do this: inserting a small, hollow tube (catheter) into the fluid-filled space in the brain (ventricle), or placing a small, hollow device (bolt) through the skull, between the skull and the brain.
There is a 2-4% risk of infection, which can lead to meningitis. Other possible complications include leg or back pain, headache, nausea, dizziness, and bleeding.
You will undergo a series of tests 3-7 days before the procedure to ensure you do not have an infection or a tendency to bleed. You should also stop taking any blood thinners and inform your doctor if you have an allergy to local anaesthetic.
After the ICP device is removed, you will need to avoid straining or lifting heavy weights for 1 week, and refrain from swimming or bathing. Contact your doctor if you experience any signs of infection or a severe headache that resolves when lying down, as this could indicate a CSF leak.