Waste anesthetic gas monitoring is essential for maintaining staff safety in various medical settings, including operating rooms, recovery rooms, dental offices, and veterinary clinics. Exposure to waste anesthetic gases (WAGs) can pose significant health risks, including nausea, dizziness, fatigue, and even more severe issues like liver and kidney disease. WAGs can escape into the surrounding environment due to leaks in anesthesia machines, defective tubing, or human errors. To ensure staff safety and comply with regulatory standards, it is crucial to perform waste anesthetic gas monitoring regularly. This involves using on-site instruments, passive dosimeter badges, and evaluating ambient air exposure to keep breathing levels within safe limits. The frequency of monitoring depends on factors such as equipment changes and seasonal variations, with OSHA recommending periodic safety surveys to be conducted at least semi-annually.
| Characteristics | Values |
|---|---|
| How often should it be performed? | OSHA recommends that waste anesthetic gas safety surveys be performed periodically, at least twice a year. |
| Who should perform the monitoring? | A reputable third-party firm that is unbiased and not involved in the anesthesia machine maintenance. |
| What is monitored? | Ambient air exposure of anesthetic agents, locations of high- and low-pressure anesthetic gas leaks, and ventilation (including air exchange rates, positive/negative pressure, and nitrous oxide (N2O) recirculation). |
| Where is it monitored? | Operating rooms, recovery rooms, dental offices, and veterinary clinics. |
| Why is it important? | To maintain staff safety, prevent occupational illness, and meet regulatory standards set by organizations such as NIOSH, OSHA, DHHS, and TJC. |
| How is it monitored? | Through on-site instruments, passive dosimeter badges worn by employees, and portable direct-reading instruments. |
| What are the potential risks of exposure? | Nausea, dizziness, fatigue, irritability, headaches, liver and kidney disease, miscarriages, sterility, birth defects, genetic damage, and cancer. |
| What are the sources of exposure? | Leaks in anesthesia machines, defective parts, human errors, exhale in recovery rooms, and poorly fitting face masks. |
| What are the recommended practices to reduce exposure? | Proper ventilation, scavenging, use of personal protective equipment, and work practice controls (e.g., avoiding unnecessary gas flow, using properly fitting masks, and disposing of waste properly). |
| What are the regulatory agencies involved? | NIOSH, OSHA, DHHS, TJC, JCAHO, ASHRAE, and AAMI. |
| What are the monitoring tools and technologies? | VAPOR-TRAK® monitoring badges, portable infrared gas analyzers, and FTIR analyzers. |
| What are the exposure limits? | Safe human exposure concentration for halogenated anesthetic agents is <50 ppm TLV or 25 ppm of nitrous oxide over an 8-hour TWA. |
What You'll Learn

Health effects of waste anesthetic gases
Waste anesthetic gases (WAGs) are a health concern for workers in operating rooms, dental offices, and veterinary clinics. WAGs are produced when anesthetic gases and vapors leak into the surrounding room during medical or research procedures. An estimated 200,000 healthcare professionals in the US alone are potentially exposed to these gases and may suffer related health issues.
WAGs can escape from the machine and into the room through leaks in various components, such as tank valves, high- and low-pressure connections, defective rubber or plastic tubing, hoses, and ventilator bellows. They can also be caused by human error, such as leaving gas flow control valves open, keeping vaporizers on after use, spilling liquid anesthetics, or using poorly fitting face masks.
The National Institute for Occupational Safety and Health (NIOSH) states that exposure to high concentrations of WAGs, even for a short time, may cause health issues including headaches, irritability, fatigue, nausea, drowsiness, difficulties with judgment and coordination, and liver and kidney disease.
Additionally, NIOSH reports that some studies have linked long-term exposure to low concentrations of WAGs to miscarriages, genetic damage, and cancer among operating-room workers. Miscarriages have also been reported in the spouses of exposed workers, and there is evidence of birth defects in their offspring. Other reported health effects of excessive exposure to WAGs include sterility, dizziness, and cancer.
To minimize the health risks associated with WAGs, healthcare facilities should employ preventative measures such as regular maintenance and repairs by an anesthesia machine technician. Health care waste anesthesia gas testing should also be conducted by a reputable third-party firm to ensure staff safety and compliance with regulatory standards.
Troubleshoot Vertical Lines on Your ASUS Monitor
You may want to see also

Preventing leaks
To prevent leaks of waste anesthetic gases, it is important to follow certain guidelines and best practices. Here are some measures that can be implemented to minimize the risk of leaks:
- Anesthesia Machine Maintenance: Regular maintenance and checks of anesthesia machines are crucial. This includes inspecting and replacing defective parts such as tank valves, high- and low-pressure connections, rubber or plastic tubing, hoses, ventilator bellows, and ventilator bellows. Qualified personnel should perform maintenance and repairs to ensure the machine is in good working order.
- Proper Work Practices: Improper practices, such as leaving gas flow control valves open, keeping vaporizers on after use, spilling liquid anesthetics, or using poorly fitting face masks, can contribute to gas leaks. It is important for healthcare professionals to be trained in proper work practices to minimize the risk of leaks.
- Scavenging Systems: The use of effective scavenging systems is essential for capturing and removing waste anesthetic gases at the source. These systems collect excess gases from the breathing circuit and safely dispose of them, preventing leaks into the surrounding environment.
- Ventilation: Adequate ventilation plays a vital role in diluting and removing waste gases. Proper ventilation systems, including general room ventilation and local exhaust ventilation, help minimize the buildup of waste gases and reduce the risk of exposure.
- Monitoring and Detection: Regular monitoring of waste anesthetic gas levels can help identify leaks and ensure the effectiveness of control measures. This includes both personal and area sampling to assess worker exposure and overall air quality.
- Personal Protective Equipment: While not a substitute for engineering and administrative controls, personal protective equipment (PPE) can provide an additional layer of protection for healthcare workers. PPE such as gloves, goggles, face shields, and chemical protective clothing can be used during cleanup and containment of spills to minimize exposure risks.
- Training and Education: Educating healthcare professionals about the risks associated with waste anesthetic gases and proper work practices is crucial. Training programs should cover topics such as equipment maintenance, leak detection, and appropriate responses to spills or leaks.
- Spill Response: In the event of a spill or leak, rapid response is essential. Absorbent materials designed for cleaning up organic chemicals should be used to contain and absorb liquid anesthetics. Proper disposal procedures should be followed, and airborne monitoring should be conducted after cleanup to ensure the effectiveness of the response.
- Engineering Controls: In addition to scavenging systems and ventilation, other engineering controls can be implemented. For example, using a machine-specific interface that integrates with the facility's gas removal system can help prevent leaks.
- Administrative Controls: Implementing policies and procedures to minimize the risk of leaks is important. This includes routine inspection and maintenance of equipment, monitoring programs to measure waste gas levels, and training programs for employees to raise awareness and promote safe work practices.
By following these measures and maintaining a proactive approach to leak prevention, healthcare facilities can significantly reduce the risk of waste anesthetic gas leaks and protect the health and safety of their staff and patients.
Best Places to Buy Monitors in Denmark
You may want to see also

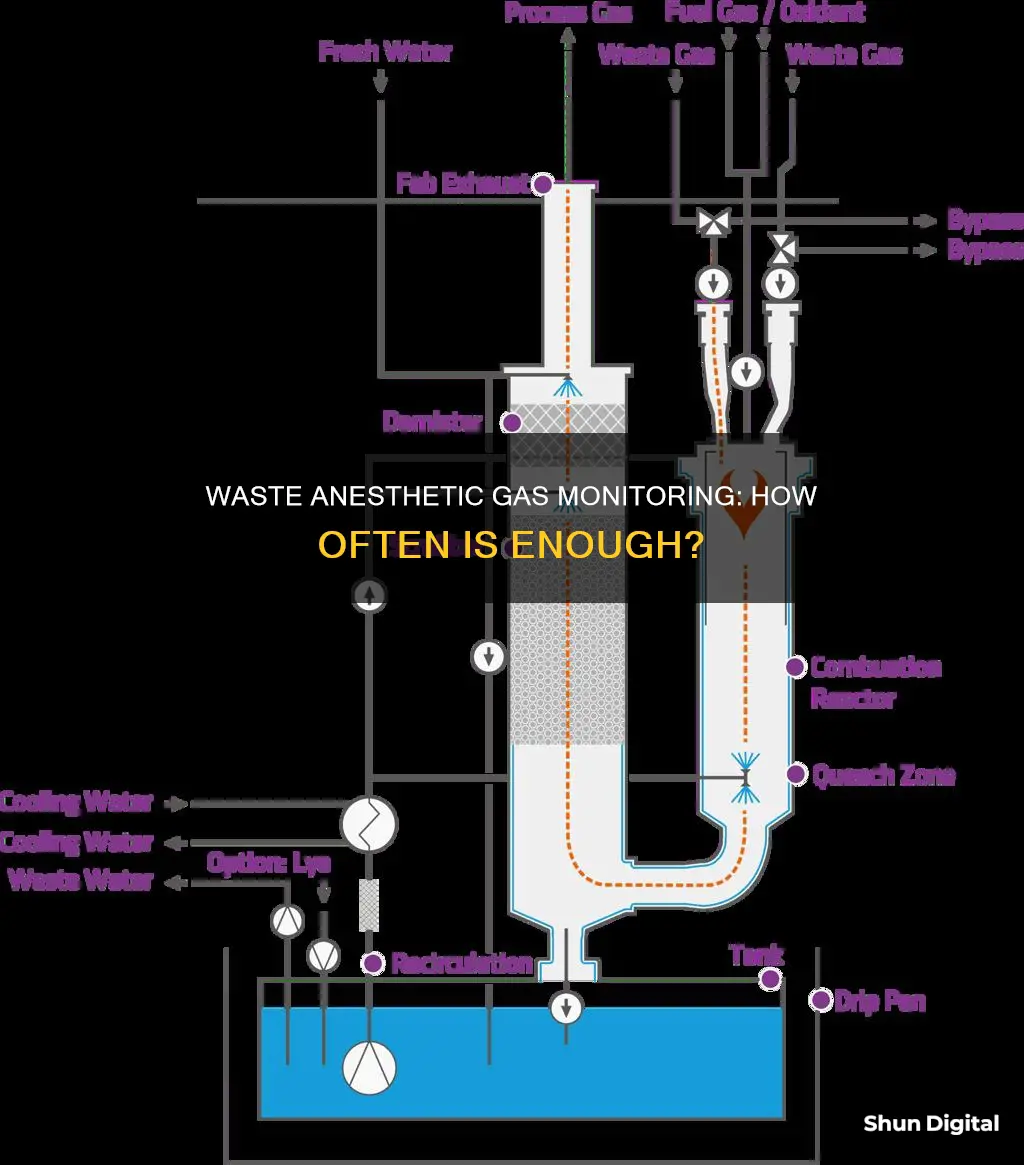
Ventilation and scavenging systems
The importance of ventilation and scavenging systems in preventing waste anesthetic gas (WAG) exposure cannot be overstated. WAGs can escape into the surrounding environment through leaks in anesthesia machines, valves, defective tubing, and even poorly fitting face masks. General building ventilation systems are insufficient to control WAGs, and specific engineering controls are necessary.
Active scavenging devices, such as nose cones, intubation, and house vacuum systems, are recommended to control WAG exposure. Passive scavenging is only suggested when active scavenging is not feasible. To ensure the effectiveness of these systems, ventilation air flow studies are conducted to determine supply and exhaust air changes, adhering to equipment manufacturer and regulatory guidelines.
In operating rooms, scavenged conditions are essential to reducing WAG exposure. Even with scavenging systems in place, operating room personnel may still be exposed to high concentrations of nitrous oxide. Therefore, managing the general ventilation system and airflow direction is crucial to lowering environmental concentrations of nitrous oxide to safer levels.
The use of snorkel exhaust, backdraft, or downdraft tables can also help control WAG exposure. Additionally, proper maintenance and repair of anesthesia machines are vital to prevent leaks and ensure ventilation requirements are met.
To summarize, effective ventilation and scavenging systems are critical in minimizing WAG exposure for healthcare professionals. Active scavenging devices, ventilation airflow management, and the use of specialized equipment all contribute to creating a safer working environment in operating rooms and healthcare facilities.
Monitoring and Managing Chromebook Usage: Tips for Parents and Teachers
You may want to see also

Monitoring methods
The monitoring of waste anesthetic gases (WAGs) is crucial to ensure the safety of healthcare professionals and prevent potential occupational illnesses. WAGs can escape into the surrounding environment through leaks in anesthesia machines, defective parts, or human error, posing a risk to those nearby. Here are some methods used to monitor and control WAGs:
Waste Anesthetic Gas Monitoring Badges:
WAG monitoring badges, such as the VAPOR-TRAK® badges, are worn by employees to collect samples of the air they breathe. These badges are then sent to a laboratory or separate analyzer for testing, with results typically taking around two weeks. While this method provides valuable data, the long turnaround time makes it challenging to identify the source of WAG exposure promptly.
Portable Gas Analyzers:
Portable gas analyzers, such as those based on Nondispersive Infrared (NDIR) or Fourier-Transform Infrared (FTIR) technology, offer faster and more versatile solutions. FTIR analyzers, in particular, can measure multiple gases simultaneously, providing a comprehensive analysis. The GT5000 Terra, for example, is a portable FTIR analyzer that can wirelessly detect up to 50 gases in real time.
On-Site Environmental Monitoring Services:
Specialized companies like Evergreen Medical Services and Kem Medical Products offer on-site WAG monitoring services. These services include measuring employee exposure levels, real-time monitoring and leak testing of anesthesia equipment, ventilation airflow studies, and providing recommendations for health and safety improvements. OSHA recommends that such safety surveys be conducted periodically, at least semi-annually, to account for equipment, procedural, personnel, or seasonal changes.
Ventilation and Scavenging Systems:
General building ventilation systems are often insufficient to control WAGs effectively. Instead, active scavenging devices, such as nose cones, intubation, or house vacuum systems, are recommended to capture and remove WAGs from the environment. Proper scavenging, along with effective ventilation, plays a vital role in minimizing WAG exposure for healthcare workers.
Work Practice Controls:
Implementing specific work practices can help reduce human exposure to WAGs. This includes proper handling of anesthesia equipment, selecting well-fitting masks, using appropriate tracheal tubes, occluding the Y-piece during surgery, and proper disposal of anesthetic waste gases into scavenging systems rather than releasing them into the room.
By employing these monitoring and control methods, healthcare facilities can help ensure the safety of their staff and comply with regulations set by organizations such as OSHA, NIOSH, and other regulatory bodies.
The Ultimate Guide to Completely Dismantling Your Monitor
You may want to see also

Regulatory standards and recommendations
In the US, waste anesthetic gas (WAG) monitoring is conducted to meet the standards set by the National Institute for Occupational Safety and Health (NIOSH), the Occupational Safety and Health Administration (OSHA), the Department of Health and Human Services (DHHS), The Joint Commission (TJC), and other regulatory agencies.
NIOSH (2007) states that exposure to high concentrations of WAGs, even for a short time, may lead to health issues such as headaches, irritability, fatigue, nausea, drowsiness, difficulties with judgment and coordination, and liver and kidney disease. Long-term exposure to low concentrations has been linked to miscarriages, genetic damage, and cancer among operating-room workers, as well as miscarriages in spouses of exposed workers and birth defects in their children.
To ensure staff safety, healthcare facilities employ an anesthesia machine technician to perform preventative maintenance and repairs, preventing gases and vapors from leaking into the room during procedures.
OSHA recommends that safety surveys be conducted periodically, taking into account equipment, procedural, personnel, or seasonal changes. It is suggested that testing be performed at least semi-annually due to the increasing emphasis on workplace exposure to toxic chemicals.
WAG monitoring is crucial to preventing serious health effects on workers in operating rooms, dental facilities, and veterinary clinics. It is estimated that over 200,000 healthcare professionals in the US alone are potentially exposed to WAGs and are at risk of occupational illness.
General building ventilation systems are inadequate to control WAGs. Instead, engineering controls such as chemical fume hoods, snorkel exhausts, or active scavenging devices should be used to reduce human exposure.
Work practice controls are also recommended to minimize human exposure to WAGs. These include:
- Avoiding turning on N2O or a vaporizer until the circuit is connected to the patient
- Switching off N2O and vaporizers when not in use
- Using the optimal size tracheal tube for the patient and ensuring the cuff is adequately inflated
- Occluding the Y-piece if the breathing circuit is disconnected during surgery
- Emptying the breathing bag into the scavenging system instead of the room after discontinuing anesthesia
- Continuing to administer anesthetic gases as long as clinically necessary, using high oxygen flow rates to wash the gases out of the system and the patient
- Closing an anesthetic circle and reducing fresh-gas flow rates
- Using properly fitting masks to minimize gas leakage and reduce waste
- Using a box for anesthesia induction in small, uncooperative patients, with tight seals and placement near the ventilation port
- Connecting the box to a scavenging system to evacuate gases before removing the patient
- Ensuring the reservoir bag is adequate to contain all scavenged gases
Air monitoring is another critical aspect of WAG management. When human exposure to WAGs is suspected, air monitoring should be conducted for both worst-case and routine exposures for each job class. Results should be reported to the supervisor and shared with the monitored workers.
Is Your Home Internet Being Watched? Here's How to Tell
You may want to see also
Frequently asked questions
Waste anesthetic gas monitoring should be performed at least twice a year to measure worker exposure and check the effectiveness of control measures.
Exposure to waste anesthetic gases can cause nausea, dizziness, fatigue, irritability, headaches, and in cases of prolonged exposure, more serious effects like liver and kidney disease, miscarriages, sterility, and birth defects.
Waste anesthetic gases can escape due to leaks in the anesthesia machine, including in tank valves, high- and low-pressure connections, defective rubber or plastic tubing, and ventilator bellows. They can also escape due to human error, such as leaving gas flow control valves open or keeping vaporizers on after use.
The National Institute for Occupational Safety and Health (NIOSH) has set a safe human exposure concentration for halogenated anesthetic agents at less than 50 parts per million (ppm) over an 8-hour time-weighted average. For nitrous oxide, the recommended exposure limit is 25 ppm.