Serum studies are an important tool in the diagnosis and monitoring of renal disorders. They can help identify the presence of renal disease, monitor the response of the kidneys to treatment, and determine the progression of renal disease.
The most common serum studies used to evaluate kidney function include:
- Serum creatinine: Creatinine is a waste product of muscle metabolism and is freely filtered by the glomeruli. It is usually produced at a constant rate, and elevated levels can indicate reduced kidney function. However, serum creatinine alone may not be a good indicator of kidney function, as it can be affected by factors such as muscle mass, diet, and certain medications.
- Blood Urea Nitrogen (BUN): Urea is a waste product of protein metabolism, and elevated BUN levels can indicate renal dysfunction. However, BUN levels can also be increased by factors unrelated to renal disease, such as high-protein diets or gastrointestinal bleeding.
- Estimated Glomerular Filtration Rate (eGFR): The eGFR is a calculation of how much blood the kidneys filter every minute and is considered the best overall indicator of glomerular function. It can be estimated using formulas based on serum creatinine and other factors.
- Urine Albumin/Creatinine Ratio: Albuminuria, or the presence of albumin in the urine, can be an early marker of kidney damage, especially in patients with diabetes. Increased levels of albumin in the urine can indicate glomerular dysfunction and are associated with an increased risk of cardiovascular disease and chronic renal impairment.
- Other Markers: Other serum studies that may be monitored in renal disorders include electrolytes (sodium, potassium, chloride), minerals (calcium, phosphorus, magnesium), and proteins (cystatin C). These markers can help assess electrolyte balance, acid-base status, and kidney function.
| Characteristics | Values |
|---|---|
| --- | --- |
| Glucose | Also known as blood sugar |
| Phosphorus | Essential mineral for bones, teeth, nervous system, and muscles |
| Calcium | Vital mineral for bones, muscles, cardiovascular system, and nervous system |
| Potassium | Electrolyte that enables acid-base balance, healthy fluid levels, and proper functioning of muscles and nerves |
| Sodium | Electrolyte that comes from diet and is largely controlled by the kidneys |
| Chloride | Electrolyte that works with other electrolytes to maintain fluid balance |
| Bicarbonate | Electrolyte that helps assess the amount of carbon dioxide in the blood |
| Albumin | Protein produced in the liver that helps maintain proper pressure in blood vessels |
| Creatinine | Waste byproduct of normal muscle activity that is removed from the blood by the kidneys |
| Blood urea nitrogen (BUN) | Waste product from protein metabolism that is removed from the blood by the kidneys |
| Anion gap | Calculation that identifies an imbalance in electrolytes |
| Estimated glomerular filtration rate (eGFR) | Evaluation of kidney function |
| Total protein | Count of all proteins in the blood |
What You'll Learn

Serum creatinine levels
Understanding Creatinine and Its Role
Creatinine is a chemical waste product that comes from creatine, a chemical made by the body. Creatine is used to supply energy to muscles. The kidneys play a vital role in removing creatinine from the blood and excreting it through urine. Therefore, creatinine levels in the blood are a key indicator of how well the kidneys are functioning. If the kidneys are not working properly, creatinine levels in the blood will increase because less creatinine is excreted in the urine.
Measuring Serum Creatinine Levels
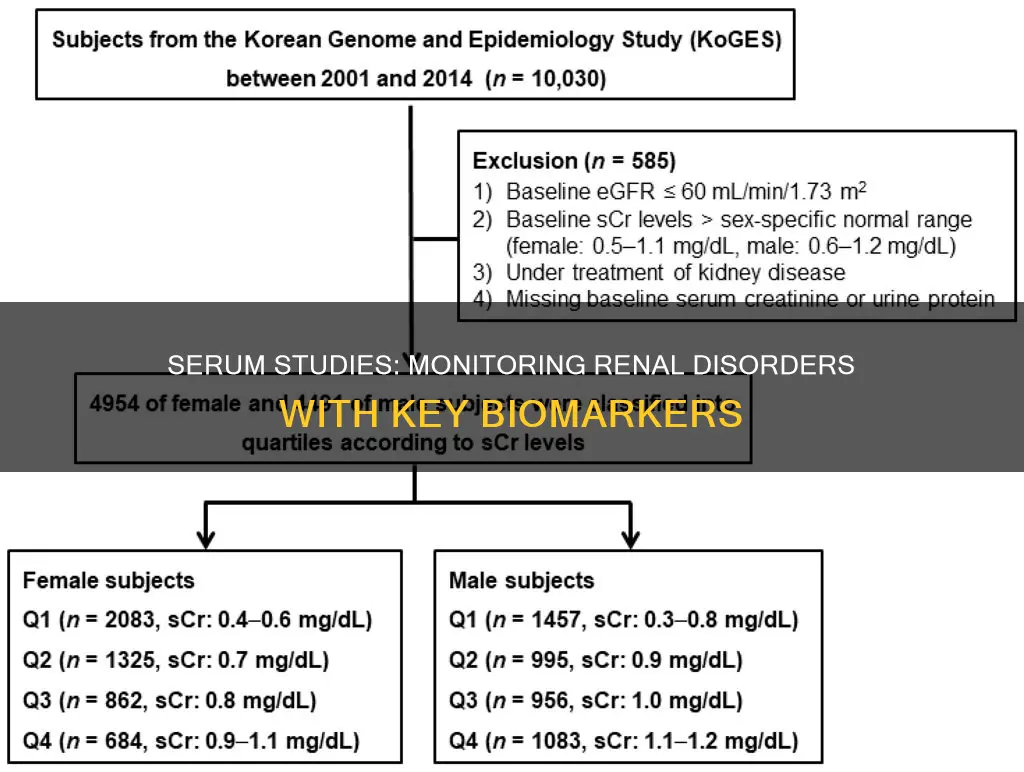
Doctors can measure serum creatinine levels through a simple blood test. This test is often used to evaluate kidney function and can help identify any issues or disorders. The normal creatinine level for men is typically between 0.7 to 1.3 mg/dL, while for women, it is usually between 0.6 to 1.1 mg/dL. It's important to note that these values can vary slightly between different laboratories.
Factors Affecting Creatinine Levels
It's important to consider that creatinine levels can be influenced by various factors. For example, women often have lower creatinine levels than men due to generally having less muscle mass. Additionally, creatinine levels can be affected by age, muscle mass, and hydration levels. Certain medications, such as antibiotics and antacids, can also impact creatinine levels, so it's important to inform your doctor about any medications you are taking.
Interpreting Creatinine Levels
High creatinine levels can indicate a range of underlying health conditions, primarily related to kidney function. If creatinine levels are above the normal range, it may suggest kidney problems such as kidney damage, infection, or reduced blood flow. Additionally, factors like dehydration, muscle breakdown, and pregnancy can also lead to elevated creatinine levels. On the other hand, low creatinine levels may be due to conditions involving muscles and nerves, resulting in decreased muscle mass.
Creatinine Levels and Kidney Function
Creatinine clearance, calculated using urine and blood creatinine levels, is used to estimate the glomerular filtration rate (GFR), which is the best overall indicator of glomerular function. GFR measures the rate at which substances are filtered through the glomerulus. Creatinine clearance should be corrected for body surface area, and improper or incomplete urine collection can affect the accuracy of this measurement. While creatinine is a widely used marker, there is a trend toward using cystatin C as a marker instead, as it is not dependent on muscle mass.
Bar's Ankle Monitor: Surveillance or Punishment?
You may want to see also

Glomerular filtration rate (GFR)
GFR specifically estimates how much blood passes through the glomeruli each minute. A GFR test is used to screen for kidney disease in people without symptoms, help diagnose kidney disease in people who are symptomatic, and determine the severity of kidney disease. It is also used to monitor the progression of kidney disease and the effectiveness of treatment.
GFR can be measured directly, but it is a complicated test, so healthcare providers usually estimate GFR based on the amount of certain waste substances in the blood. An estimated GFR is called an eGFR. The standard way to estimate GFR is with a simple blood test that measures creatinine levels. Creatinine is a waste product that comes from the digestion of dietary protein and the normal breakdown of muscle tissue.
To calculate eGFR, a blood sample is sent to a lab where the creatinine level in the blood is tested. The lab specialist combines the blood creatinine level with several other factors to estimate GFR. Different formulas are used for adults and children.
An eGFR of 90 or higher is in the normal range, while an eGFR of 60-89 may indicate early-stage kidney disease. An eGFR of 15-59 may indicate kidney disease, and an eGFR of below 15 may indicate kidney failure.
GFR is classified into several stages based on kidney disease. Stage 1 CKD refers to patients with a normal GFR but other signs of possible renal structural damage, such as proteinuria. Stage 2 CKD is a GFR of 60 to 89 mL/min/1.73 m², and stage 3 CKD is a GFR of 45 to 59 mL/min/1.73 m². Stage 4 CKD is a GFR of 15 to 29 mL/min/1.73 m², and stage 5 CKD (end-stage renal disease) is a GFR less than 15 mL/min/1.73 m².
Simple Ways to Check Your Monitor's Refresh Rate
You may want to see also

Blood urea nitrogen (BUN)
A BUN test measures the amount of urea nitrogen in the blood. It is often part of a comprehensive metabolic panel (CMP) and can help diagnose or monitor kidney diseases. A small amount of urea nitrogen in the blood is normal, but higher-than-normal levels may indicate that the kidneys are not functioning correctly.
BUN levels can be affected by factors other than kidney function. For example, BUN levels can vary according to age, sex, diet, and hydration status. BUN levels are often combined with creatinine levels to obtain the BUN-to-creatinine ratio, which can help determine renal failure.
High BUN levels may be caused by:
- Impaired kidney function
- High-protein diet
- Dehydration
- Congestive heart failure
- Increased protein breakdown due to gastrointestinal bleeding, trauma, or corticoid therapy
Low BUN levels may be caused by:
- Low-protein diet
- Malnutrition or starvation
- Overhydration
- Pregnancy
- Liver disease
If high BUN levels are caused by kidney disease, treatment may include managing any underlying disorders and treating complications. In severe cases, dialysis or a kidney transplant may be necessary. Low BUN levels are generally not a cause for concern and may not require treatment.
Best Places to Buy BP Measure X Monitor
You may want to see also

Serum cystatin C
In patients with acute kidney injury (AKI), serum creatinine levels do not increase until a moderate to severe reduction in GFR occurs, which can delay detection of kidney damage and therapeutic interventions. In contrast, serum cystatin C levels start to rise early in AKI and can help identify early kidney dysfunction that may be missed by relying on serum creatinine alone. Serum cystatin C is also useful in detecting early nephropathy in diabetic patients, as it may be elevated even before the onset of clinical albuminuria.
However, serum cystatin C levels can be affected by factors such as cancer, thyroid disease, and smoking. Additionally, older age has been associated with higher serum cystatin C levels, even after adjusting for creatinine clearance. Therefore, while serum cystatin C is a valuable tool for monitoring renal function, particularly in the early stages of AKI, it should be interpreted in conjunction with other clinical factors and laboratory findings.
Removing Sticker Residue from Your Monitor: A Quick Guide
You may want to see also

Urine albumin/creatinine ratio
The urine albumin/creatinine ratio (ACR) is a simple urine test that is used to identify kidney disease, particularly in people with diabetes.
ACR is the ratio of albumin, a protein normally found in the blood, to creatinine in the urine. When the kidneys are functioning properly, only tiny amounts of albumin pass from the bloodstream into the urine. However, if the kidneys are damaged, protein can "leak" out of the kidneys and into the urine. This is called albuminuria or proteinuria.
A normal amount of albumin in the urine is less than 30 mg/g. A level above 30 mg/g may indicate kidney disease, even if other tests show no abnormality. A high ACR may be an early sign of kidney disease, but further testing is needed to rule out other causes. Two high results over three months or more is a sign of kidney disease.
The ACR test is typically requested when diabetes is first diagnosed and then measured annually or more frequently if the level is high. It can also be used to monitor kidney function over time in people with diabetes or hypertension.
In addition to ACR, other tests that may be done to evaluate kidney function include imaging (such as ultrasound or CT scan), kidney biopsy, and blood tests such as the estimated glomerular filtration rate (eGFR) and serum creatinine level.
FL Studio on External Monitor: Setup Guide
You may want to see also
Frequently asked questions
A renal function test is a series of tests that examine how well the kidneys are working in removing waste products (urea, toxins, uric acid) and extra water from the blood (urine) and ensuring proper balance of key chemical elements such as sodium, potassium, calcium, etc. They also help in producing certain hormones that are necessary in the production of red blood cells, maintaining blood pressure, and bone development.
The different types of renal function tests include serum creatinine level, urine, blood, and imaging tests (e.g., ultrasonography, CT, MRI).
The symptoms of renal disorders include hematuria, unexplained swelling, loss of concentration, difficulty breathing, nausea and/or vomiting, muscle cramps or pain, etc.
The risk factors for renal disorders include high blood pressure, diabetes, and a family history of kidney disease.
Renal function is monitored through regular blood tests for urea and electrolytes. The frequency of monitoring depends on the patient's condition and medication. It is recommended to monitor renal function every 6 months for stable patients, and more frequently (ranging from days to 2 weeks) if there are changes in the drug regimen.