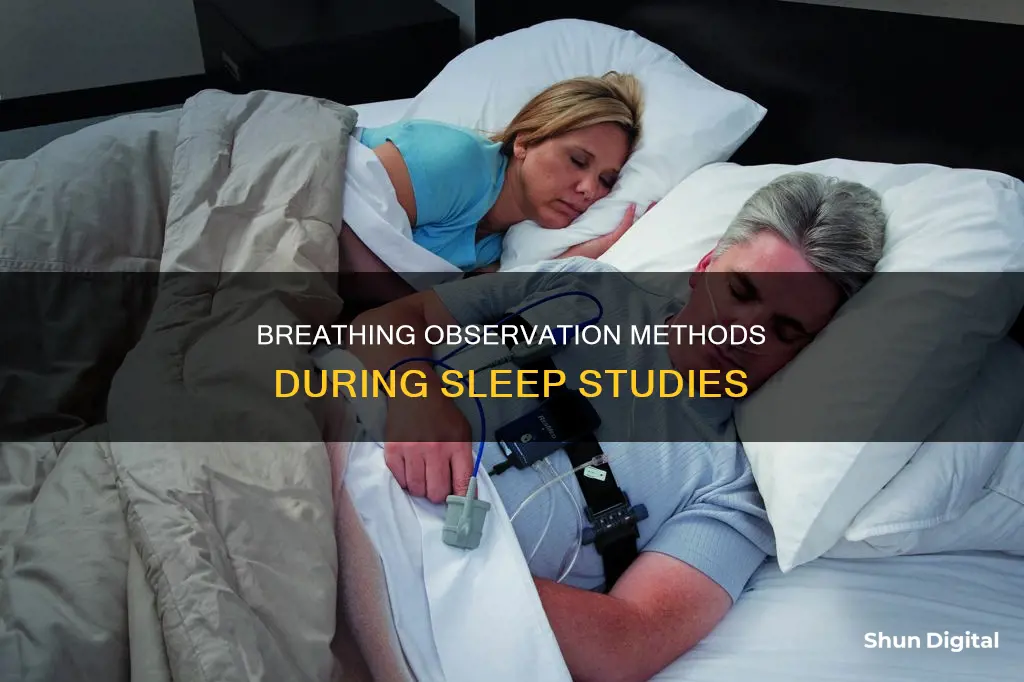
Sleep studies are diagnostic tests that monitor multiple body systems, including brain activity, heart function, and breathing, to identify sleep-related conditions. Breathing is monitored through various methods, such as sensors, elastic belts, pulse oximeters, and audio or video recordings. These tools track respiratory activity, oxygen levels, and chest movement to detect issues like sleep apnea and other sleep disorders.
| Characteristics | Values |
|---|---|
| Sensors | Electroencephalography (EEG), Electrocardiography (EKG or ECG), Electromyogram (EMG), Electro-oculography (EOG), Breathing sensors, Respiratory inductive plethysmography (RIP) belt, Pulse oximeter |
| Monitoring methods | Video and audio monitoring |
What You'll Learn

Sensors that detect breathing through the nose and mouth
Sleep studies are diagnostic tests that involve recording multiple systems in the body while a person sleeps. Sensors are used to track the activity of multiple body systems, including the heart, brain, and respiratory system.
During a sleep study, breathing sensors are used to detect air movement through the nose and mouth. These sensors are attached to the skin with adhesive and connected to a computer to record data. These sensors can also be used in at-home sleep studies, which are often used to detect sleep apnea.
At-home sleep studies typically involve a small probe placed over the finger to measure oxygen levels, as well as a mask with tubes inserted into the nostrils to measure breathing patterns. Sensors are also placed on the abdomen and chest to measure their rise and fall as the person breathes.
In a sleep lab, elastic belts may be wrapped around the chest and abdomen to measure breathing. A clip may also be placed on the finger or earlobe to monitor oxygen levels in the bloodstream.
For people who breathe through their mouths at night, there are also devices such as chin straps and mouth tape that can be used to prevent this and encourage nasal breathing.
Monitoring Packet Usage: A Guide for Windows 10 Users
You may want to see also

Pulse oximeter
A pulse oximeter is a small adhesive sensor that is placed on the tip of the index finger to monitor pulse and blood oxygen levels during a sleep study. It is a simple test that can be done at home to provide basic information about sleep disorders like sleep apnea. The device shines a red light through the finger or skin surface, and a sensor on the other side measures the pulse and oxygen content of the blood. The colour of the blood, which varies depending on the amount of oxygen it contains, changes the frequency of the light wavelength reflected back to the sensor.
The pulse oximeter is connected to a small box that records data overnight, or it can be connected to a continuous positive airway pressure (CPAP) device to record data. Newer devices may adhere directly to the skin and provide similar measurements. The data is recorded continuously throughout the night and is presented in a graph format. A pulse oximeter can detect abnormal drops in oxygen levels, which may indicate a condition called hypoxemia. Levels below 88% indicate hypoxemia, and desaturations below 80% are considered severe.
The pulse oximeter is a useful tool for evaluating sleep disorders and lung conditions, but it has limitations. It does not take into account sleep position and sleep stages, which can impact oxygen levels. Therefore, additional tests, such as polysomnography, may be required for a comprehensive diagnosis.
The pulse oximetry device can be worn on the wrist or as a finger sensor. It is designed to be comfortable and soft, allowing the finger to move freely. Some devices offer multi-user management, allowing health information for up to 10 family members to be managed. The data can be seamlessly synced to an app or PC software for in-depth analysis, and it can be integrated with Apple Health to provide daily feedback. The device has a rechargeable battery with a battery life of up to 16 hours and can operate independently without a smartphone.
Blind Spot Monitor: A Camry Safety Feature?
You may want to see also

Respiratory inductive plethysmography (RIP) belt
Respiratory inductive plethysmography (RIP) is a method of evaluating pulmonary ventilation by measuring chest and abdominal wall movements. It is a non-invasive technique that uses two elastic belts with embedded sensors to monitor breathing during sleep studies. These belts are placed around the torso, with one positioned just below the rib cage and the other just above the stomach. This positioning allows for the capture of both diaphragm and chest breathing.
The RIP method offers several advantages over traditional devices such as masks or mouthpieces. It does not require direct coupling to the airway opening, making it more comfortable and less intrusive for patients. RIP is particularly useful for continuous or ambulatory measurements as it does not restrict the patient's movements.
The belts contain sinusoidal wire coils that generate a magnetic field using alternating current (AC). During breathing, the cross-sectional area of the rib cage and abdomen changes, altering the self-inductance of the coils and the frequency of their oscillation. This change in frequency is then converted into a digital respiration waveform, where the amplitude of the waveform is proportional to the inspired breath volume.
RIP is often combined with other respiratory sensors, such as nasal/oral airflow sensors, to provide a comprehensive assessment of respiratory function. It is widely used in clinical settings and academic research, including sleep studies (polysomnography), psychophysiology, psychiatry, and cardiology, among others.
In the context of sleep studies, RIP belts provide valuable data on respiratory effort and flow limitation. They help detect conditions such as sleep apnea and determine their origin (central vs. obstructive). Additionally, RIP allows for the evaluation of ventilation parameters such as tidal volume, inspiratory and expiratory times, and their subsequent ratios, providing insights into bulbar respiratory control centres.
Viewing HDMI and DVI on Your ASUS Monitor
You may want to see also

Polysomnography
PSG monitors several body functions, including brain activity (using electroencephalography or EEG), eye movements (electro-oculography or EOG), muscle activity or skeletal muscle activation (electromyography or EMG), and heart rhythm (electrocardiography or ECG). After the identification of sleep apnea in the 1970s, breathing functions, respiratory airflow, and respiratory effort indicators were added to PSG, along with peripheral pulse oximetry.
During a PSG, sensors are attached to the patient's head and body with adhesive to track the activity of multiple body systems. Elastic belts may be wrapped around the chest and abdomen to measure breathing efforts, and a clip may be placed on the finger or earlobe to monitor blood oxygen levels. The patient's brain activity and selected body information are recorded while they sleep, providing a detailed picture of their unique sleep patterns.
PSG can directly monitor and quantify the number of respiratory events and the resultant hypoxemia and arousals related to these events. It can also be used to evaluate abnormalities of sleep and/or wakefulness and other physiological disorders that impact sleep and wakefulness. PSG data can be related to sleep onset latency, REM sleep onset latency, the number of awakenings during sleep, total sleep duration, and the number of arousals.
PSG is considered the criterion standard for diagnosing obstructive sleep apnea syndrome (OSAS) and is commonly used for this purpose. A single-night PSG is usually adequate to determine the presence and degree of OSAS. However, home-based, limited-channel sleep studies are becoming more common for diagnosing OSAS due to their lower cost and convenience, although they have some limitations.
Disabling GamePlus on Your ASUS Monitor: A Simple Guide
You may want to see also

At-home sleep tests
At-home sleep apnea tests are portable breathing monitors that you wear overnight. They are designed to help diagnose OSA by monitoring your breathing and oxygen levels to detect and measure pauses in breathing, known as apneas. The test calculates an OSA severity score by calculating the average number of lapses in breathing per hour in bed.
Most at-home sleep apnea tests measure:
- Respiratory activity, breathing patterns, and chest motion
- Heart rate and blood oxygen level
- Nocturnal movement and motor activity
- Sleep position and position changes
- Snoring events and intensity
At-home sleep apnea tests do not measure sleep quality, so they may be limiting if you are trying to decide between an at-home test or an onsite sleep study. Polysomnography, an overnight sleep study performed in a lab, provides a more holistic overview of your sleep quality and sleep patterns, in addition to the apnea-related metrics measured by at-home tests.
To obtain an at-home sleep apnea test, you will need a prescription from your doctor. The test will cost between $100 to $500, compared to a laboratory test, which can cost thousands of dollars. The test will be delivered to your doorstep, and you will typically use it for just one night. After the test, a sleep specialist will interpret the results and send them to your doctor.
While at-home sleep apnea tests offer many benefits, there are some drawbacks to consider. They may be less accurate than monitored lab tests, and there is a risk of technological malfunctions, such as sensors falling off during the night. Additionally, at-home tests only monitor breathing and oxygen levels, whereas overnight sleep studies monitor more vitals related to sleep, including brain waves and leg and eye movements.
Removing a ViewSonic Monitor Stand: A Step-by-Step Guide
You may want to see also
Frequently asked questions
A sleep study, also known as a polysomnogram, is a diagnostic test that tracks and records the activity of multiple body systems, including the heart, brain and respiratory system, to give healthcare providers a comprehensive view of the quality of an individual's sleep.
After arriving at the sleep centre, a technician will apply small sensors to the patient's head and body with adhesive. The sensors will track eye activity, brain activity, muscle movement, heart rate, blood oxygen levels, leg and arm movements, and breathing.
There are in-lab sleep studies and at-home sleep studies. In-lab sleep studies are considered the gold standard for diagnosing sleep apnea, as they capture many more signals, including brainwaves, muscle tone and leg movements. At-home sleep studies are a more affordable and convenient option, but they are not suitable for everyone.
Breathing is monitored during a sleep study using breathing sensors that detect air movement through the mouth and nose. A respiratory inductive plethysmography (RIP) belt may also be used to detect the expansion of the torso when the patient breathes.