Intracranial pressure monitoring is performed when there is a life-threatening neurological emergency, such as severe head trauma, brain surgery, brain infection, hydrocephalus, brain tumours, or other problems that may cause brain swelling. It is also used to monitor patients with traumatic brain injuries, intracranial hypertension, and cerebral perfusion pressure. The procedure involves inserting a device inside the head to sense and measure the pressure inside the skull.
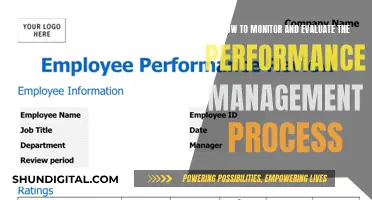
| Characteristics | Values |
|---|---|
| Normal ICP range | 7-15 mm Hg |
| ICP range in vertical position | Does not exceed 15 mm Hg |
| ICP lowering therapy initiation | ICP exceeds 20-25 mm Hg |
| ICP monitoring methods | Intraventricular catheter, subdural screw (bolt), epidural sensor |
| ICP monitoring indications | Severe head injury, brain/nervous system disease, brain swelling, hydrocephalus, brain tumours, intracranial hypertension, traumatic brain injury, CSF circulatory disorders |
| ICP monitoring contraindications | Concurrent use of anticoagulant drugs, coagulopathies, anti-coagulation medication, scalp infections, brain abscess |
What You'll Learn
- Intracranial pressure monitoring is used to treat severe head injuries
- It can also be used after surgery to fix damage to a blood vessel
- It is performed on people with life-threatening neurological emergencies
- It is also used to treat hydrocephalus
- Intracranial monitoring is recommended for patients with traumatic brain injury

Intracranial pressure monitoring is used to treat severe head injuries
Intracranial pressure (ICP) monitoring is a procedure that involves inserting a device inside the skull to measure the pressure inside. It is usually performed on patients with life-threatening neurological emergencies, such as severe head injuries, brain/nervous system diseases, brain tumours, or post-surgery to remove a tumour. ICP monitoring is crucial in preventing permanent damage or death resulting from high ICP.
ICP monitoring is recommended for patients with a Glasgow Coma Scale score of less than 8 and those with abnormal CT scan results showing conditions such as mass lesions, brain swelling, or compressed basal cisterns. It is also indicated for patients with hydrocephalus or conditions that can develop into hydrocephalus, such as subarachnoid haemorrhage. Additionally, ICP monitoring can be considered for patients with bifrontal contusions, respiratory failure, or unreliable neurological examinations due to maxillofacial trauma or spinal cord injury.
The procedure can be performed in two ways: through an intraventricular catheter or a subdural screw (bolt). The intraventricular catheter method, considered the most accurate, involves drilling a hole through the skull and inserting a catheter into the lateral ventricle of the brain, which contains cerebrospinal fluid (CSF). The subdural screw method, on the other hand, is used when immediate monitoring is required. It involves inserting a hollow screw through a hole drilled in the skull and into the subdural space.
ICP monitoring helps guide treatment decisions by providing continuous data on ICP levels. When ICP levels exceed the normal range of 7 to 15 mm Hg, therapeutic interventions can be initiated to lower ICP. These interventions may include draining CSF through the catheter, adjusting ventilator settings for patients on a respirator, or administering specific medications intravenously.
ICP monitoring plays a crucial role in the management of severe head injuries by helping to avoid potentially harmful aggressive treatments. By closely monitoring ICP, healthcare professionals can make informed decisions to optimise patient outcomes and safety.
Portable Monitors: Worth the Investment?
You may want to see also

It can also be used after surgery to fix damage to a blood vessel
Intracranial pressure monitoring is a procedure that uses a device placed inside the head to sense the pressure inside the skull and relay measurements to a recording device. This procedure is often carried out on patients with life-threatening neurological emergencies.
Intracranial pressure monitoring can be performed after surgery to fix damage to a blood vessel if the surgeon is concerned about brain swelling. This procedure can help to avoid permanent damage caused by high intracranial pressure.
There are three methods of intracranial pressure monitoring:
- Intravenous Catheter: This is considered the most accurate monitoring method. A hole is drilled through the skull, and a catheter is inserted through the brain into the lateral ventricle, which contains cerebrospinal fluid (CSF). The CSF is a liquid that protects the brain and spinal cord. The catheter can also be used to drain out excess CSF.
- Subdural Screw (Bolt): This method is used when immediate monitoring is required. A hollow screw is inserted through a hole drilled in the skull and placed through the membrane that protects the brain and spinal cord (dura mater). This allows the sensor to record from inside the subdural space.
- Epidural Sensor: This procedure is less invasive than the other methods but cannot remove excess CSF. A sensor is inserted between the skull and the dural tissue through a hole drilled in the skull.
The procedure is usually carried out in the hospital intensive care unit, and the patient's health care provider will explain the procedure and its risks. The patient will also need to sign a consent form.
Intracranial pressure monitoring can help guide treatment decisions, such as draining CSF, changing ventilator settings, or administering medications to reduce intracranial pressure and prevent potential harm to the brain.
Safety Performance Monitoring: Measurement Strategies and Techniques
You may want to see also

It is performed on people with life-threatening neurological emergencies
Intracranial pressure (ICP) monitoring is a procedure performed on people with life-threatening neurological emergencies. It involves inserting a device inside the head to sense and measure the pressure inside the skull. This procedure is crucial for patients with severe head injuries, brain/nervous system diseases, or post-surgery complications to prevent permanent damage or death.
ICP monitoring is typically performed in intensive care units, with the patient's consent, and can be done under general or local anaesthesia. The procedure involves drilling a hole into the skull and inserting a catheter or a screw into the brain to measure the pressure. ICP monitoring helps guide treatment decisions, such as draining cerebrospinal fluid, adjusting ventilator settings, or administering medications.
The normal ICP range is between 1 to 20 mm Hg, and pressures above 20 mm Hg often indicate the need for treatment. ICP monitoring is an essential tool for managing life-threatening neurological emergencies and guiding interventions to prevent further harm.
Ankle Monitors: Texas Crimes and Consequences
You may want to see also

It is also used to treat hydrocephalus
Intracranial pressure monitoring is a procedure that involves placing a device inside a person's head to measure the pressure inside their skull. This procedure is often performed on patients with life-threatening neurological emergencies, such as severe head injuries, brain tumours, or hydrocephalus.
Hydrocephalus is a condition where there is a build-up of cerebrospinal fluid (CSF) in the brain, which can lead to increased intracranial pressure. The CSF is a liquid that protects the brain and spinal cord. In cases of hydrocephalus, intracranial pressure monitoring can help detect and manage this increased pressure, reducing the risk of permanent damage or life-threatening complications.
The monitoring procedure can be done in two ways: by inserting a small, hollow tube (catheter) into the fluid-filled space in the brain (ventricle) or by placing a small, hollow device (bolt) through the skull, between the skull and the brain. These devices are connected to a monitor that provides a constant reading of the intracranial pressure.
If the pressure increases significantly, it can be treated promptly by draining the CSF through the catheter, changing ventilator settings for patients on a respirator, or administering specific medications.
The decision to perform intracranial pressure monitoring is typically made when a patient is in the hospital intensive care unit. The procedure is usually carried out when the benefits of monitoring and potential treatment outweigh the risks of the procedure itself, which can include brain herniation, brain tissue damage, and infection.
In the context of hydrocephalus, intracranial pressure monitoring plays a crucial role in managing the condition and preventing further complications. By closely monitoring the intracranial pressure, healthcare professionals can make informed decisions about drainage of CSF, administration of medications, and other therapeutic interventions to maintain optimal cerebral perfusion pressure and reduce the risk of permanent brain damage.
Finding Your Monitor Model: A Simple Guide
You may want to see also

Intracranial monitoring is recommended for patients with traumatic brain injury
Intracranial pressure (ICP) monitoring is a procedure that involves placing a device inside the head to measure the pressure inside the skull. This procedure is often performed on patients with life-threatening neurological emergencies, such as severe head injuries, brain/nervous system diseases, or brain swelling after surgery. It is particularly recommended for patients with traumatic brain injuries (TBIs) and is considered the cornerstone of TBI management.
ICP monitoring is important because high ICP can lead to permanent damage or even death if left untreated. By monitoring ICP, healthcare providers can detect elevated ICP early and intervene with appropriate treatments to lower ICP. These treatments may include draining cerebrospinal fluid (CSF) through a catheter, changing ventilator settings for patients on a respirator, or administering certain medications intravenously.
The decision to perform ICP monitoring is typically made when a patient is in the hospital intensive care unit (ICU) and is based on the patient's condition and risk factors. ICP monitoring is generally recommended for patients with a Glasgow Coma Scale score of less than 8 and those with abnormal computed tomography (CT) scans of the head. It may also be recommended for patients with certain risk factors, such as age over 40, unilateral or bilateral motor posturing, or systolic blood pressure below 90 mmHg.
There are several methods for ICP monitoring, including invasive and non-invasive techniques. The most accurate and commonly used method is the intraventricular catheter, where a catheter is inserted through a hole drilled in the skull into the lateral ventricle of the brain, which contains CSF. This method also allows for the drainage of CSF to reduce ICP. Another method is the subdural screw or bolt, which is less invasive and involves inserting a hollow screw or bolt through the skull and the membrane protecting the brain and spinal cord. This method does not allow for CSF drainage.
ICP monitoring is a valuable tool in the management of TBIs, as it provides critical information to guide medical and surgical therapies. It helps prevent and manage secondary brain injuries, such as cerebral ischemia and intracranial hypertension, which can significantly impact patient outcomes.
While ICP monitoring is generally recommended for patients with TBIs, there are some considerations and potential complications. For example, ICP monitoring may not be recommended for comatose patients with initial normal CT scans or only minor findings. Additionally, there are risks associated with the procedure, including brain herniation, brain tissue damage, infection, and technical issues.
In summary, ICP monitoring is a crucial aspect of managing patients with TBIs. It provides essential information to guide treatments aimed at reducing ICP and improving patient outcomes. The decision to perform ICP monitoring is based on the patient's condition and risk factors, and it involves various techniques to measure ICP accurately.
ASUS Monitor Drivers: Where Are They Stored?
You may want to see also
Frequently asked questions
Intracranial pressure monitoring is performed on a child when there is a severe brain injury, head surgery, brain infection, or other problems that may cause the brain to swell.
Intracranial monitoring is performed on a patient with a tumour when there is a risk of cerebral edema or raised intracranial pressure.
Intracranial monitoring is performed on a patient with a head injury when there is a risk of intracranial hypertension.