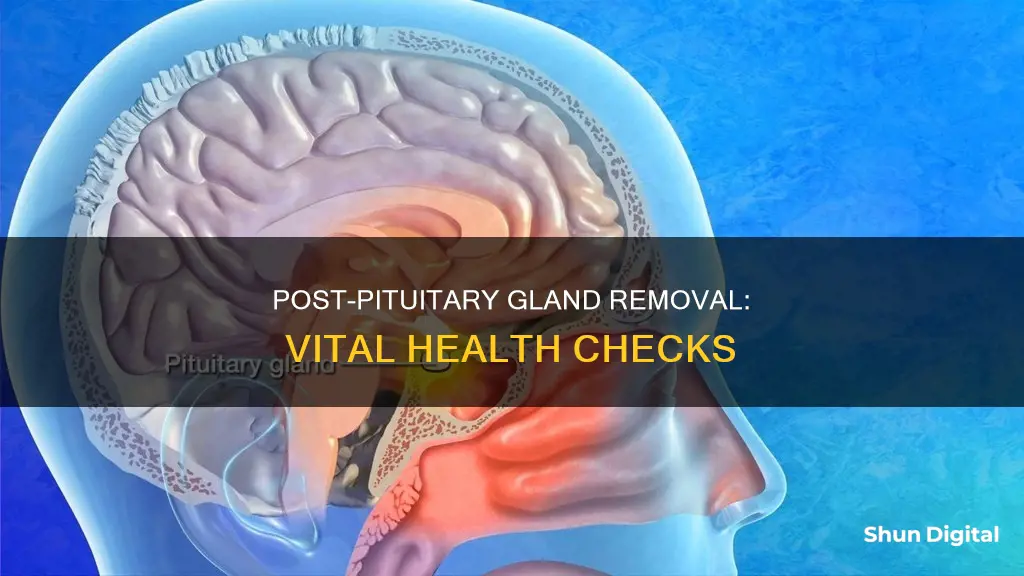
Following pituitary gland removal, patients should be aware of the possibility of other hormone deficiencies, depending on how much of the pituitary was removed. Hormone replacement may be necessary for thyroid, estrogen, progesterone, and growth hormones. In patients with diabetes insipidus, desmopressin (DDAVP) is needed to prevent excessive urination and thirst.
In the immediate aftermath of surgery, patients will likely experience headaches and discomfort, as well as nasal congestion and a sore nose. It is important to avoid blowing your nose for at least two weeks after surgery, and to avoid sneezing if possible.
In the first few weeks, patients may feel fatigued and should pace themselves, slowly increasing their activity and resting when tired. It is also recommended to sleep with the head elevated to decrease pain and swelling.
In terms of medication, patients may be placed on Prednisone or Dexamethasone, and it is important to continue taking this medication until instructed to stop. Patients should also be aware of the signs of high or low blood sodium, which can be caused by the pituitary gland not releasing enough of the hormone that regulates sodium levels.
In the longer term, patients should be aware of potential improvements or deterioration in their senses of smell and taste. It is also important to continue seeing an endocrinologist to monitor hormone production and adjust medication as necessary.
| Characteristics | Values |
|---|---|
| Hormone levels | Cortisol, ACTH, thyroid hormone, estrogen, progesterone, growth hormone |
| Vital signs | Blood pressure, pulse, temperature |
| Urine output and fluid intake | Monitored to check for diabetes insipidus |
| Blood sodium levels | Monitored to check for hypernatremia or hyponatremia |
| Vision | May be impaired post-surgery |
| Recovery time | 2-4 weeks of fatigue, with overall recovery time depending on the individual |
What You'll Learn
Monitor sodium levels in the blood
Following pituitary surgery, it is crucial to monitor sodium levels in the blood to prevent abrupt variations and maintain homeostasis. This monitoring is essential because disorders of water metabolism, such as diabetes insipidus, syndrome of inappropriate antidiuretic hormone secretion (SIADH), and the rare cerebral salt-wasting syndrome, can occur post-operatively. These disorders can lead to either high or low blood sodium levels, which require careful management.
High blood sodium levels, or hypernatremia, can result from diabetes insipidus, where the pituitary gland fails to release adequate amounts of the hormone regulating sodium levels. This condition can cause excessive urination and extreme thirst, with patients awakening multiple times at night to drink. To address this, blood tests are regularly conducted in the first two weeks after surgery to monitor sodium and hormone levels. If hypernatremia is detected, medication may be prescribed to control urination and thirst until the pituitary gland resumes normal function, typically within several days.
On the other hand, low blood sodium levels, or hyponatremia, can be indicative of SIADH. In this case, the pituitary gland releases excessive amounts of the hormone regulating sodium levels. Symptoms of hyponatremia include nausea without a fever. As with hypernatremia, regular blood tests in the initial two weeks post-surgery are crucial for detecting hyponatremia. If left untreated, severe hyponatremia can lead to seizures. Therefore, patients exhibiting severe symptoms such as confusion, lethargy, or an inability to stay awake should seek immediate medical attention. Treatment for hyponatremia may include a fluid-restricted diet until the pituitary gland recovers its normal function.
The monitoring of sodium levels in the blood is a critical aspect of post-pituitary surgery care. By closely observing these levels, healthcare professionals can identify and manage potential complications arising from disorders of water metabolism. This proactive approach ensures the well-being and recovery of patients following pituitary gland removal.
Blind Spot Monitor: How Does It Work?
You may want to see also
Check for CSF leaks
Checking for CSF Leaks after Pituitary Gland Removal
Cerebrospinal fluid (CSF) leaks are a possible complication of pituitary gland removal surgery. They occur when a defect develops in the coverings of the brain, often as a result of cranial trauma, skull base tumours, or prior skull base surgery. Given the potential risk of meningitis and other neurological complications, it is essential to urgently and effectively repair the skull base defect.
Symptoms of a CSF Leak
If a CSF leak is left untreated, it can lead to a potentially dangerous infection of the CSF (meningitis) or brain (brain abscess). Therefore, it is important to be vigilant for any symptoms of a CSF leak after pituitary gland removal surgery.
A CSF leak is usually associated with watery clear drainage out of the nose (after endonasal surgery) or out of a surgical incision. If there is persistent drainage occurring within the first 1-2 weeks after surgery, you should contact your surgeon promptly.
Other symptoms of a CSF leak include:
- Headache
- Stiff neck
- Fever
- Photophobia (sensitivity to light)
- Weakness
- In-coordination
- Confusion
Diagnosis of a CSF Leak
The diagnosis of a CSF leak is typically made by noting watery drainage out of the nose or a surgical incision. To confirm the presence of CSF, a sample of the fluid can be collected and tested for Beta-2 transferrin, a compound found only in CSF.
In some cases, a brain MRI or CT scan may be performed to identify the location of the leak and determine if there is any intracranial air (pneumocephalus). A CT scan with injection of a contrast agent through the lumbar spine (a spinal tap) can also help localise the origin of the leak.
Treatment of a CSF Leak
The treatment of a CSF leak requires either direct surgical repair or, in some cases, the temporary diversion of CSF through a lumbar drain or ventriculostomy (a catheter placed in the ventricle of the brain). In certain situations, both surgical repair and CSF diversion may be necessary to effectively seal the leak.
Prevention of CSF Leaks
The technique of covering the sella membrane and dural defects with Surgicel and TachoSil during surgery has been shown to be effective in preventing postoperative CSF leaks. This method involves using regenerated oxidised cellulose and a collagen sponge with human fibrin to cover the defects, followed by packing the sella with autologous fat.
Vertical Monitors: Optimal Viewing Sizes for Comfort
You may want to see also
Monitor for signs of meningitis
Following the removal of the pituitary gland, it is important to monitor for signs of meningitis. Meningitis is a serious condition that can develop alongside septicaemia, and both conditions can worsen very quickly. Therefore, it is important to be vigilant and seek medical help immediately if you are concerned.
Meningitis and septicaemia can affect people of any age and have similar symptoms, which can appear in any order. These may include:
- Fever with cold hands and feet
- Drowsiness or difficulty waking someone
- Confusion and irritability
- Pale, blotchy skin, spots, or a rash that does not fade under pressure or when a glass is rolled over it
- Dislike of bright lights
- Convulsions or seizures
- Stiffness or floppiness
- High-pitched crying
- Bulging soft spot on the head (in babies)
In addition, specific symptoms in babies may include:
- Being very sleepy
- Being unresponsive
- Having a high-pitched cry
It is important to note that some of these symptoms may not appear at all, and a rash may not always be present or may be difficult to see on darker skin tones. However, it is crucial not to wait for a rash to develop before seeking medical help. If you or someone you are caring for is displaying any of these symptoms, trust your instincts and seek medical assistance immediately.
Understanding Monitor Types: A Guide to Identifying Your Display
You may want to see also
Check for damage to the pituitary gland
Checking for damage to the pituitary gland after surgery is crucial to ensure the patient's safety and well-being. Here are some detailed instructions and guidelines to monitor and manage potential complications:
Hormone Deficiencies
It is important to monitor the patient for potential hormone deficiencies, as the extent of pituitary gland removal can impact hormone production. Other hormone replacements may be necessary, such as thyroid hormone, estrogen, progesterone, and growth hormone. Blood tests are essential to assess thyroid function, measuring free T4 and TSH levels. For pre-menopausal women, it is advisable to wait 3-4 months post-surgery to observe if menstrual cycles return before considering estrogen and progesterone replacement. Growth hormone deficiency may require stimulation tests such as arginine or insulin tests to diagnose.
Diabetes Insipidus
Diabetes Insipidus (DI) is a potential complication that can arise due to disturbances in water regulation caused by surgical injury to the hypothalamus or posterior pituitary gland. It is characterised by inappropriate hypotonic polyuria and normal or high serum sodium levels. DI can be transient or permanent, and its occurrence can vary from 10-30% of patients, with only 2-7% persisting long-term. Monitoring urine output, fluid intake, urine specific gravity, and serum sodium levels is crucial to detect DI early. Treatment options include short-acting subcutaneous vasopressin or desmopressin (DDAVP).
Syndrome of Inappropriate Antidiuretic Hormone (SIADH)
SIADH is another possible complication, characterised by excessive ADH release leading to water retention. It typically occurs 5-8 days post-surgery and is more common in patients with cardiac, renal, or thyroid disease, older age, and low body mass index. Monitoring for signs and symptoms of SIADH, such as hyponatremia, is crucial. Treatment focuses on fluid restriction, and severe cases may require hospitalisation with hypertonic saline or ADH receptor antagonist drugs.
Cerebral Salt-Wasting Syndrome (CSWS)
CSWS is a rare complication characterised by excessive natriuresis and extracellular volume depletion. It is essential to differentiate CSWS from SIADH, as they have distinct management approaches. CSWS is managed with hypertonic fluid administration, while SIADH is optimally treated with fluid restriction. Weight, serum osmolality, protein levels, and hematocrit can aid in the differential diagnosis.
Visual Impairment
Visual impairment after pituitary surgery is rare but possible. It can be caused by direct surgical damage or postoperative compression of optic structures by haemorrhage in the surgical bed. If visual impairment occurs, early detection and prompt referral to an ophthalmologist are crucial for further evaluation and management.
Hormone Replacement Therapy
Hormone replacement therapy may be initiated before or after surgery, depending on the patient's condition. It is essential to closely monitor hormone levels and adjust medications accordingly. Patients should be instructed on how to increase their medication dosage during illness or stress.
Long-Term Follow-Up
Long-term follow-up is crucial to assess pituitary function and hormone production. Endocrinological assessments, including blood tests and stimulation tests, may be performed at regular intervals to monitor hormone levels and adjust replacement therapies accordingly. Additionally, follow-up MRI or CT scans may be scheduled to evaluate the pituitary gland's condition and detect any regrowth of the tumour.
Patient Education
Educating patients about potential complications and providing them with clear instructions is essential. Patients should be advised to contact their healthcare team if they experience any unusual symptoms, such as persistent headaches, nasal discharge, or changes in vision. Additionally, providing information about self-care practices, activity restrictions, and when to resume normal activities can aid in their recovery.
Identifying 10-Bit Monitors: What to Look For
You may want to see also
Monitor for diabetes insipidus
Diabetes insipidus is a common complication following pituitary gland removal, and it can be transient or permanent. It is defined by a constellation of signs and symptoms resulting in dilute high-volume urine output and increasing serum osmolality. The body's inability to concentrate urine leaves the patient dehydrated and leads to metabolic abnormalities that can be life-threatening if not recognised and treated in a timely manner with an exogenous vasopressin analogue.
The reported incidence of post-surgical central diabetes insipidus varies from 1 to 67%. This wide range likely reflects inconsistencies in the working definition of diabetes insipidus across the literature. Factors affecting the rate of diabetes insipidus include pituitary tumour size, adherence to surrounding structures, surgical approach, and histopathology of the pituitary lesion. The likelihood of postoperative diabetes insipidus can be reduced by careful preservation of the neurovascular structures of the hypothalamus, infundibulum, and neurohypophysis. Vigilance and meticulous surgical technique are essential to minimising injury to these critical regions, which can lead to post-surgical diabetes insipidus.
The onset of polyuria is usually abrupt, occurring within the first 12-24 hours after surgery. However, it is important to note that polyuria may not always be due to diabetes insipidus; it can also be caused by the mobilisation of intraoperative fluids, hyperglycaemia, or the use of certain medications such as furosemide or SGLT2 inhibitors. Therefore, documentation of hypotonic polyuria is essential in establishing the diagnosis of diabetes insipidus.
The diagnosis of post-pituitary surgery diabetes insipidus could be challenging due to several factors, including the lack of universal diagnostic criteria and enormous variability in the monitoring of patients following pituitary surgery. Moreover, the current diagnostic criteria may not apply to patients who are able to consume water and self-manage diabetes insipidus, especially if the condition is partial.
The treatment of diabetes insipidus is typically multifaceted and should be individualised for every patient. The goal of treatment is to maintain and/or restore osmotic equilibrium. The acute phase management covers the first two phases of the triphasic water dysregulation phenomenon. The management is straightforward, provided there is an intact thirst mechanism, i.e. the patient is not receiving fluids for any reason and can drink water at will. Water balance can be achieved under such a situation as long as the patient can consume enough fluids.
Vasopressin is available as an aqueous solution and should be administered through IV infusion when acute control of antidiuresis is needed. Infusion is usually started at a rate of 0.25-1.0 micro units/kg/h and titrated every half hour after that to maintain the urine output rate at around 100 mL/h and/or urine specific gravity at around 1.010-1.020.
Desmopressin (DDAVP) is a synthetic analogue of vasopressin, having a prolonged action profile with minimal vasopressor activity. It can be administered orally, intranasally, subcutaneously, or intravenously. Studies have shown a definite relationship between the magnitude and duration of its therapeutic effect and its IV dosage. In patients with diabetes insipidus, 1 μg IV 'push' infusion can increase urine osmolality to a maximum of 700-800 mOsmol/kg. Further increase in dose, from 1 to 8 μg, led to prolongation of the duration of action from around 26 hours to 46 hours. The magnitude and duration of its therapeutic effects showed large interindividual variability attributed to individual differences in renal concentration abilities.
The management of diabetes insipidus in specific populations, such as neonatal infants/children, pregnancy and lactation, and the elderly, may require special considerations. For example, in the elderly, there is a higher risk of developing hyponatremia, primarily when intranasal DDAVP is used. The aetiology is unclear, but it may be due to abnormalities of osmoregulation of thirst and fluid intake, along with increased renal sensitivity to DDAVP.
Setting Up Stage Monitor Speakers: A Comprehensive Guide
You may want to see also
Frequently asked questions
Clear fluid leaking from the nose or frequently swallowing salty liquid from the back of the throat are signs of a cerebrospinal fluid (CSF) leak. This is a rare but serious complication that requires immediate medical attention.
High blood sodium, or hypernatremia, may cause excessive urination and extreme thirst, such as awakening multiple times at night to urinate. This can be a temporary condition called diabetes insipidus, which can occur when the pituitary gland doesn't release enough of the hormone that regulates sodium levels.
Symptoms of low blood sodium, or hyponatremia, may include nausea, vomiting, and severe cases can cause confusion, lethargy, and an inability to stay awake. This can be caused by the pituitary gland releasing too much of the hormone that regulates sodium levels.
It is recommended to avoid heavy lifting, straining, and strenuous exercise for at least the first two weeks post-surgery. Swimming with the head below water should be avoided for three months due to the risk of infection. Driving is not advised while taking narcotic pain medication, and flying is generally not recommended for the first six weeks.







